It is H2 heading of the page.
It is H3 heading of the page.
It is H4 heading of the page
A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
- hello this is the list of page
- hello this is the list of page
Here is another list:
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page

Respiratory Emergencies: Causes, Symptoms, and When to Call for Help
Respiratory emergencies are sudden failures of the airway, breathing, or oxygenation that can rapidly cause hypoxia and death. Early recognition and immediate first aid improve survival.
Recognizing the warning signs, such as difficulty breathing, low oxygen levels, or inability to speak, is critical for timely intervention and better outcomes. This article explains common respiratory emergencies. It shows why getting BLS certification from the American Training Association for CPR can help you respond well.
.avif)
What are Respiratory System Emergencies?
Respiratory system emergencies are sudden problems. They make breathing, oxygen exchange, or airway opening worse. Quick recognition is vital to prevent hypoxia, organ damage, and systemic collapse.
Respiratory failure develops through one or more mechanisms:
- Airway obstruction – from tongue fallback, foreign body, facial or neck trauma, or swelling due to anaphylaxis. In the lower airway, asthma or COPD flare-ups often cause bronchospasm.
- Failure of ventilation – when chest wall or respiratory muscles cannot generate effective breaths. This can result from rib fractures, flail chest, or neuromuscular disorders like Guillain-Barré syndrome.
- Failure of gas exchange – when oxygen transfer in the lungs breaks down, such as with pulmonary edema, ARDS, pneumonia, or massive pulmonary embolism.
- Loss of neural control – when the brain fails to regulate breathing.
.avif)
Each can reduce oxygen uptake and raise carbon dioxide. Symptoms can include rapid breathing, confusion, cyanosis, and respiratory distress. Without treatment, patients may progress to respiratory failure, cardiovascular collapse, or death.
What are the Common Types of Respiratory Emergencies?
Respiratory emergencies come in many forms, but they share one thing in common: they require immediate recognition and action. Below are the most common types, their warning signs, and urgent responses.
1. Asthma Attacks
Asthma attacks occur when the airways suddenly narrow due to bronchospasm and inflammation. Signs include wheezing, chest tightness, coughing, and difficulty speaking in full sentences. Severe cases may lead to confusion or exhaustion as oxygen levels drop. Quick treatment with inhaled bronchodilators and prompt medical care are vital to prevent respiratory failure.
2. Choking and Airway Obstruction
Choking happens when food, objects, or swelling block airflow, making it difficult or impossible to breathe. Victims may be unable to speak or cough, show stridor, turn blue, or make silent attempts to breathe. Immediate action is crucial: according to the American Red Cross, abdominal thrusts for adults and children, back blows and chest thrusts for infants, and CPR if the person becomes unresponsive.
3. Anaphylaxis and Severe Allergic Reactions
Anaphylaxis is a life-threatening allergic reaction that, according to the Centers for Disease Control and Prevention (CDC), can quickly swell the airway and cause breathing difficulties. Symptoms include swelling of the lips, tongue, or throat, hives, wheezing, stridor, dizziness, or sudden collapse. Suspected anaphylaxis is a medical emergency. Give intramuscular epinephrine immediately (preferably in the mid-outer thigh) and activate EMS; additional care follows.
.avif)
4. COPD Exacerbations
COPD flare-ups present with worsening breathlessness, cough, and sputum change. Provide short-acting bronchodilators, titrate oxygen, and assess for steroids and non-invasive ventilation when indicated; target oxygen saturation is typically 88–92% for patients at risk of hypercapnia.
Severe cases may confuse carbon dioxide buildup. Oxygen therapy and inhaled bronchodilators are important. A medical evaluation is also needed. Some patients need steroids or assisted ventilation.
5. Respiratory Infections Leading to Distress
Pneumonia and certain upper-airway infections (e.g., epiglottitis, bacterial tracheitis) can progress quickly and require urgent evaluation, oxygen support, and airway monitoring, especially in children.
CPR and FIRST AID
Certification





6. Respiratory Arrest or Failure
Respiratory arrest happens when breathing stops or does not work well. This stops oxygen delivery completely. Signs include absent or gasping breaths, no chest rise, cyanosis, and unresponsiveness.
If there is no normal breathing and no pulse, begin CPR and use an AED as soon as available. If there is a pulse but breathing is absent or inadequate, provide rescue breaths: adults 1 breath every 6 seconds; children/infants 1 breath every 2–3 seconds. Reassess every 2 minutes.
7. Pediatric and Infant Emergencies
Children and infants are especially vulnerable because of their smaller airways and limited reserves. Signs of respiratory distress include nasal flaring, chest retractions, head bobbing, grunting, or poor feeding. Stridor with drooling may signal severe upper airway obstruction. Using airway maneuvers that fit the person's age is important. Getting emergency care early helps prevent quick worsening.
Recognizing Signs of Respiratory Distress
Respiratory distress refers to the observable signs that a patient is struggling to breathe effectively. These indicators vary by age and severity, but early recognition is critical for timely intervention. Key categories of signs include:
- Breathing rate and pattern: Rapid, shallow breaths, very slow respirations, or pauses in breathing (apnea) suggest impaired ventilation. In adults, rates consistently above 20 breaths per minute raise concern, while normal ranges are higher in children (up to 30/min) and infants (up to 50–60/min).
- Airflow sounds: Wheeze indicates lower airway narrowing (e.g., asthma), stridor points to upper airway obstruction, and gurgling suggests fluid or secretions. These sounds can be more pronounced in infants due to smaller airways.
- Skin color and perfusion: Cyanosis (blue lips/tongue), pallor, or mottling reflect poor oxygenation. In darker skin tones, the lips, tongue, and oral mucosa are more reliable for assessment. These changes often signal severe hypoxemia and require urgent action.
- Accessory muscle use and posture: Signs such as nasal flaring, intercostal retractions, abdominal breathing, or the tripod position indicate increased effort to breathe. Children and infants often show more pronounced nasal flaring and retractions.
- Level of consciousness: Agitation, lethargy, or confusion often appear as oxygen levels drop and signal worsening respiratory compromise.
- Other symptoms: Persistent cough, weak cry in infants, or inability to speak full sentences in adults are additional red flags.
Recognizing these signs quickly allows responders to judge severity, prioritize care, and intervene before distress progresses to respiratory failure.
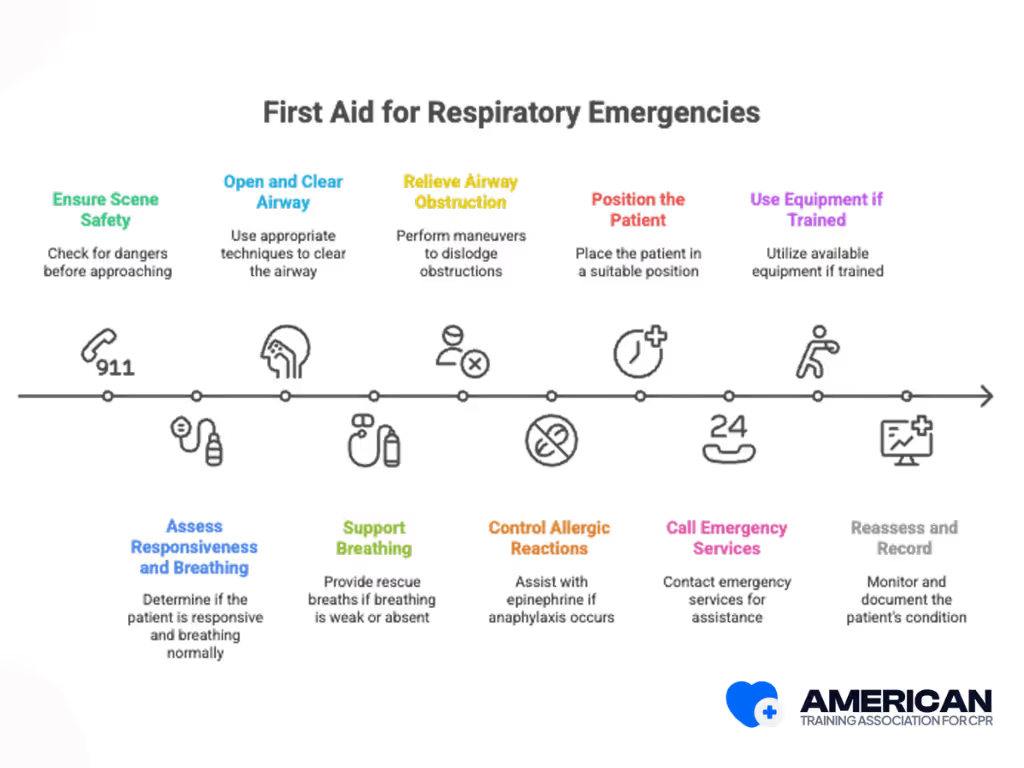
First Aid for Respiratory Emergencies
Quick, prioritized actions can maintain breathing, keep the airway clear, and buy time until emergency services arrive. Below are 10 essential steps for responding to respiratory emergencies.
- Ensure the scene is safe: Check for dangers like traffic, fire, or hazardous materials. Only approach if safe. Move the patient only if necessary.
- Assess responsiveness and breathing: Tap the patient and call out. Look, listen, and feel for normal breathing for up to 10 seconds. If absent or abnormal, treat as respiratory arrest.
- Open and clear the airway: Use head tilt–chin lift (if no spinal injury) or jaw thrust (if suspected spinal injury). Remove visible obstructions only—never do blind sweeps.
- Support breathing: If breathing is weak or absent, give rescue breaths with a barrier device. Adults: 1 breath every 6 seconds. Children/infants: 1 breath every 2–3 seconds. Ensure chest rise.
- Relieve airway obstruction: If choking, perform age-appropriate maneuvers: abdominal thrusts for adults, chest thrusts for pregnant/obese, and 5 back blows + 5 chest thrusts for infants. Start CPR if unresponsive.
- Control allergic reactions: If signs of anaphylaxis appear (swelling, wheezing, collapse), assist with an epinephrine auto-injector if available. Call EMS immediately.
- Position the patient: Sit conscious patients upright. Place unconscious but breathing patients in the recovery position. Protect the spine if trauma is suspected.
- Call emergency medical services: If distress is severe, breathing stops, or anaphylaxis occurs, dial your local emergency number. Give clear details and continue first aid until help arrives.
- Use equipment if trained: If trained, use a pocket mask, bag–valve–mask, or oxygen. Two rescuers are best for bag–valve–mask ventilation. Don’t attempt advanced airways if untrained.
- Reassess and record: Recheck breathing and responsiveness every 1–2 minutes. Note times, interventions, and changes to report to emergency responders.
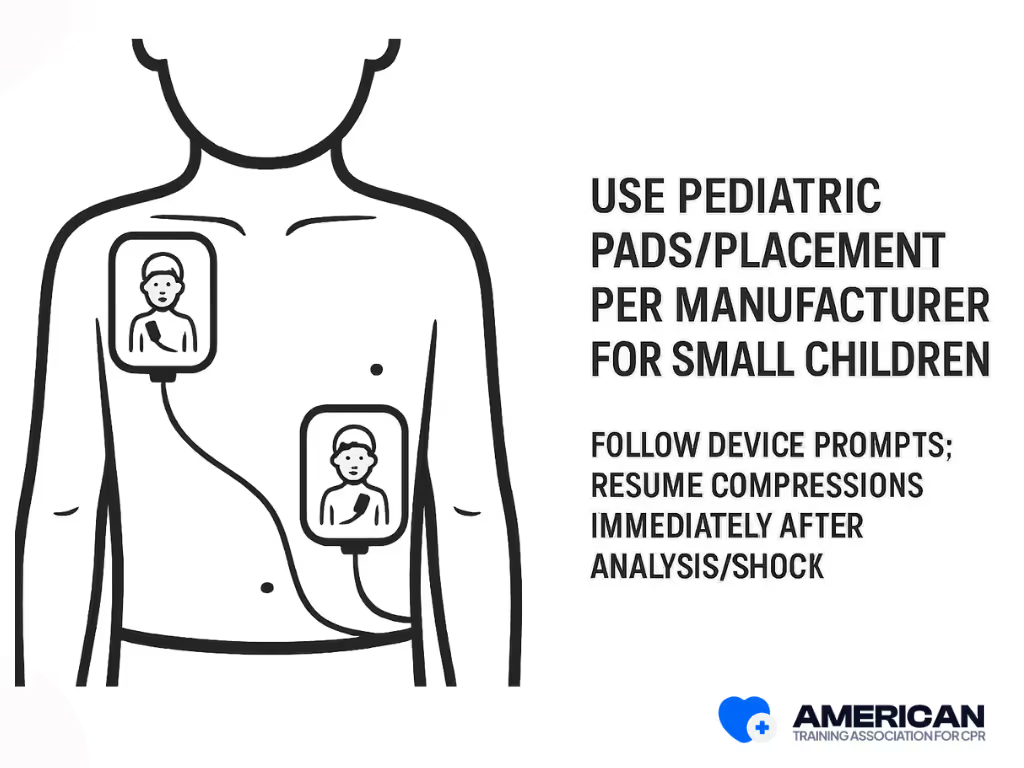
When Should You Use an AED in a Respiratory Emergency?
Use an AED as soon as cardiac arrest is suspected. Follow the device prompts. Place pads anterolaterally (one pad upper right chest, the other on the lower left chest). Resume CPR immediately after each analysis/shock. For untrained bystanders of a collapsed teen/adult, Hands-Only CPR (chest compressions without breaths) is recommended; give rescue breaths when trained or when arrest is likely asphyxial (e.g., drowning, overdose, pediatric). Use pediatric pads for small children when available.
What special considerations come up when respiratory emergencies involve chronic conditions?
Chronic diseases change how breathing emergencies look and how they should be treated. They can make symptoms appear different, cause unusual medication effects, and require unique action plans. This means responders must compare the patient’s current state with their usual baseline rather than assuming “typical” signs.
Common Chronic Conditions Affecting Breathing Emergencies
Some common chronic conditions that affect breathing emergencies include:
- COPD (emphysema, chronic bronchitis)
- Asthma (allergic, exercise-induced)
- Cystic fibrosis
- Interstitial lung disease (pulmonary fibrosis, sarcoidosis)
- Heart failure
- Neuromuscular disorders (ALS, muscular dystrophy)
.avif)
Why are personalized action plans important?
Action plans list a person’s normal symptoms, usual oxygen levels, medicines, and emergency steps. They help responders make faster, safer decisions. For example, an asthma or COPD action plan may guide when to use rescue inhalers or when to call 911.
Responders should know the names, doses, and last use of:
- Inhalers (bronchodilators, anticholinergics)
- Steroids (like prednisone)
- Blood thinners
- Oxygen flow rate or use of CPAP/BiPAP machines
When should care be escalated quickly?
With chronic conditions, responders should call for advanced help sooner if:
- Oxygen drops 3–5% below the patient’s normal baseline
- Breathing becomes harder or the person can’t speak well
- Mental status changes (confusion, drowsiness)
- Rescue inhalers or treatments don’t improve symptoms
When Should You Call Emergency Services for a Respiratory Emergency?
Not all breathing problems need an ambulance, but some symptoms are serious warning signs that require immediate medical help. Knowing when to call emergency services can save a life.
Call emergency services right away if you notice any of these signs:
- Severe shortness of breath: The person is struggling to breathe, cannot finish sentences, or is breathing too fast or too slow. According to the Centers for Disease Control and Prevention (CDC), these are clear warning signs of a respiratory emergency.
- Gasping or choking: Sudden airway blockage can quickly cause collapse if not treated. The American Red Cross notes that prompt action, such as abdominal thrusts or back blows, is critical in these situations.
- Blue lips, face, or fingertips: This is a sign of dangerously low oxygen levels, according to the American Lung Association, Signs of Hypoxia and Respiratory Distress.
- Confusion, extreme sleepiness, or unconsciousness: These changes often mean the brain isn’t getting enough oxygen. Based on guidance from the American Lung Association, altered mental status is a serious warning sign of hypoxia.
- Very rapid breathing that doesn’t stop: Especially if it comes with chest pain, fever, or low oxygen readings. According to the National Institutes of Health (NIH), persistent fast breathing may signal a severe respiratory infection or distress.
If you’re unsure, use this quick check:
- Can the person speak full sentences?
- Are they using extra muscles to breathe (neck or chest straining)?
- Is oxygen below 92% in adults (or below age-specific levels in children and infants)?
If the answer points to worsening breathing or oxygen levels, don’t wait. Call emergency services immediately
ATAC’s Recommendations for Preventing Respiratory Emergencies
Preventing respiratory emergencies means protecting your lungs, reducing risks, and staying prepared. ATAC recommends the following steps:
- Follow healthy routines: Get enough rest, drink water, eat nutritious meals, and exercise regularly. Quit smoking or vaping since they damage your lungs and increase your risk of emergencies.
- Keep your airways clear: Practice breathing exercises like diaphragmatic and pursed-lip breathing. Use nasal rinses if you have frequent congestion to keep airways open.
- Avoid environmental triggers: Stay away from smoke, pollution, and chemical irritants. Use air filters at home, and check the local Air Quality Index before going outside.
- Manage chronic conditions: If you have asthma, COPD, or other lung problems, follow your doctor’s action plan. Take medicines as prescribed and attend regular check-ups.
- Stay updated on vaccines: Get flu shots every year, and follow CDC recommendations for pneumococcal and COVID-19 vaccines to lower your risk of serious infections.
- Limit allergen exposure: Reduce dust mites, pollen, or pet dander at home. Wash bedding often, keep humidity low, and use allergen-proof covers if needed.
- Be prepared for emergencies: Keep rescue inhalers or epinephrine injectors up to date. Make sure family members know how to use them and when to call emergency services.
- Seek medical care early: Contact your doctor right away if your breathing worsens, if you need your inhaler more often, or if you develop fever with breathing problems.
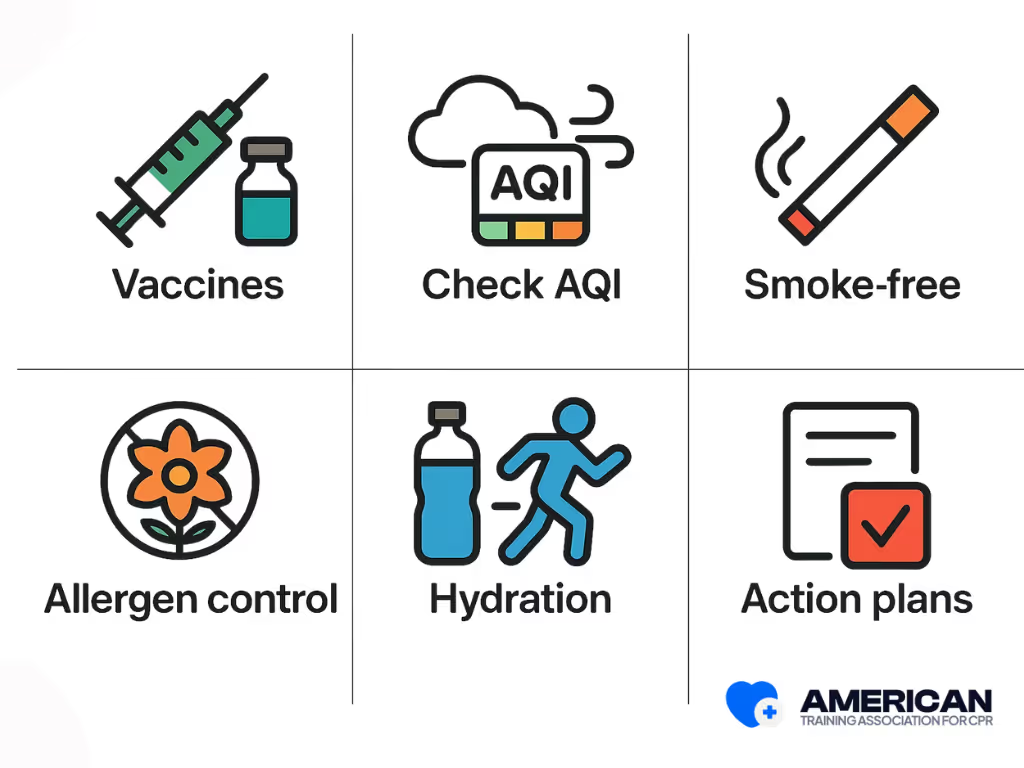
By following ATAC’s recommendations, you can reduce your risk of respiratory emergencies and protect your long-term lung health.
Workplace Preparedness for Respiratory Emergencies
Workplace preparedness for respiratory emergencies means having clear policies, proper equipment, trained staff, and a culture of safety. This includes written response plans, first aid kits, AEDs, oxygen supplies, and annual training with drills. Doing regular risk assessments helps readiness. Communication systems also help. Including all employees in measures makes readiness stronger. Routine audits and equipment checks keep everything reliable. Together, these steps help workplaces respond quickly and effectively to respiratory emergencies, reducing harm and saving lives.
.avif)
CPR and FIRST AID
Certification





When does a breathing problem become an emergency?
A breathing problem is an emergency if the person is breathing very fast or very slow, looks like they are struggling, makes noisy sounds (like wheezing, gurgling, or stridor), turns blue or gray, or cannot talk in full sentences. Call emergency services right away and help keep their airway open while waiting for help.
How do EMTs respond to respiratory emergencies?
Emergency medical technicians (EMTs) quickly check the airway, breathing rate, and oxygen levels. They may give oxygen, use breathing support devices, and decide if advanced airway care or rapid transport to the hospital is needed.
What should I do if someone is choking?
For responsive adults and children who cannot cough, speak, or breathe: alternate 5 back blows with 5 abdominal thrusts until the object is expelled or the person becomes unresponsive. For infants under 1 year: give 5 back blows followed by 5 chest thrusts. If unresponsive, start CPR and follow dispatcher/AED prompts.
How are breathing emergencies different in children?
Infants and young children may show early warning signs like poor feeding, grunting, nasal flaring, or head bobbing. They can get worse faster than adults. Call pediatric-capable emergency services immediately if you notice these signs.
Can a breathing emergency cause cardiac arrest?
Yes. Severe breathing problems can lower oxygen in the blood, which may slow or stop the heart. Fast recognition and giving oxygen or rescue breathing can prevent this.
What is Basic Life Support?
Basic Life Support is the foundation of emergency care for cardiac and respiratory arrest. It includes cardiopulmonary resuscitation (CPR), chest compressions, and airway management to keep oxygen and blood flow moving until advanced life support arrives.
CPR and FIRST AID
Certification





What does the American Heart Association recommend for chest compressions and ventilation ratio?
The American Heart Association (AHA) emphasizes high-quality chest compressions with a compression rate of 100–120 per minute and full chest wall recoil. For most adults, the recommended compression-to-ventilation ratio is 30:2, even for lay rescuers (American Heart Association, 2020 Guidelines for CPR and Emergency Cardiovascular Care).
According to the 2025 AHA Guidelines, rescuers should minimize interruptions in compressions to less than 10 seconds and use real-time feedback tools when available to improve compression rate and depth. The new updates also emphasize continuous chest compressions if ventilation is not possible, particularly for untrained bystanders.
For healthcare providers, maintaining proper coordination during team-based resuscitation and ensuring early defibrillation are key priorities. The AHA continues to stress that high-quality chest compressions are the most important factor in improving survival rates during cardiac arrest.
How do bystander CPR and the use of an automated external defibrillator improve survival?
Bystander CPR helps maintain blood flow to vital organs, while an AED can restore a normal heart rhythm. Early CPR and defibrillation are critical links in the BLS Chain of Survival, especially before EMS systems or first responders arrive.
Why is high-quality CPR important for first responders and healthcare workers?
Doing high-quality chest compressions helps survival during emergencies. Managing the airway properly also helps. Using the correct ventilation ratios improves survival too. For first responders, mastering these skills ensures they can deliver effective emergency cardiovascular care until advanced life support is available.
What role do the American Red Cross and American Academy of Pediatrics play in BLS/CPR training?
Both the American Red Cross and the American Academy of Pediatrics support BLS/CPR for healthcare providers and lay rescuers. They provide training that covers airway management, bag-mask device use, and skills sessions for pediatric and adult care.
ATAC offers an online BLS certification that is flexible and complete. It is a good choice for busy professionals. It provides convenience and follows American Heart Association guidelines. You can train on your own schedule.
Real Stories from Our BLS Certified Participants













