It is H2 heading of the page.
It is H3 heading of the page.
It is H4 heading of the page
A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
- hello this is the list of page
- hello this is the list of page
Here is another list:
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page

Ventricular Fibrillation: Symptoms, Causes, and Emergency Treatment
Ventricular fibrillation is a chaotic heart rhythm that stops effective contractions, causing sudden cardiac arrest. Immediate action with chest compressions and defibrillation is critical, as survival drops 7–10% for each minute without intervention. Understanding this condition is essential for anyone trained in Basic Life Support (BLS)
What is Ventricular Fibrillation?
Ventricular fibrillation (VF) is a life-threatening ventricular arrhythmia that stops effective heart contractions and causes immediate hemodynamic collapse. It is characterized by chaotic electrical activity in the ventricular myocardium, which prevents coordinated contraction and eliminates cardiac output.
The electrical disturbance comes from rapid, disorganized reentrant circuits or focal impulses. Reentrant circuits often form in areas of scar tissue or ischemia, while focal impulses originate from ventricular cells with abnormal membrane potentials. This chaos prevents synchronized heartbeats and causes the heart to stop pumping effectively.
VF quickly leads to sudden cardiac arrest. The brain can begin suffering injury within about 4 minutes of absent blood flow, with irreversible damage likely after 10 minutes if circulation is not restored. Immediate high-quality CPR can partially preserve perfusion until defibrillation is available.
Ventricular Fibrillation vs Ventricular Tachycardia
Ventricular fibrillation differs from ventricular tachycardia in that ventricular fibrillation produces chaotic, uncoordinated ventricular electrical activity with no effective cardiac output while ventricular tachycardia produces rapid but often organized ventricular depolarizations that may generate some cardiac output; the distinction between a chaotic, nonperfusing ventricular rhythm and an organized, potentially perfusing ventricular tachyarrhythmia matters at the bedside because it determines whether a rescuer prioritizes immediate defibrillation or assesses for a carotid pulse and performs tailored basic life support actions.
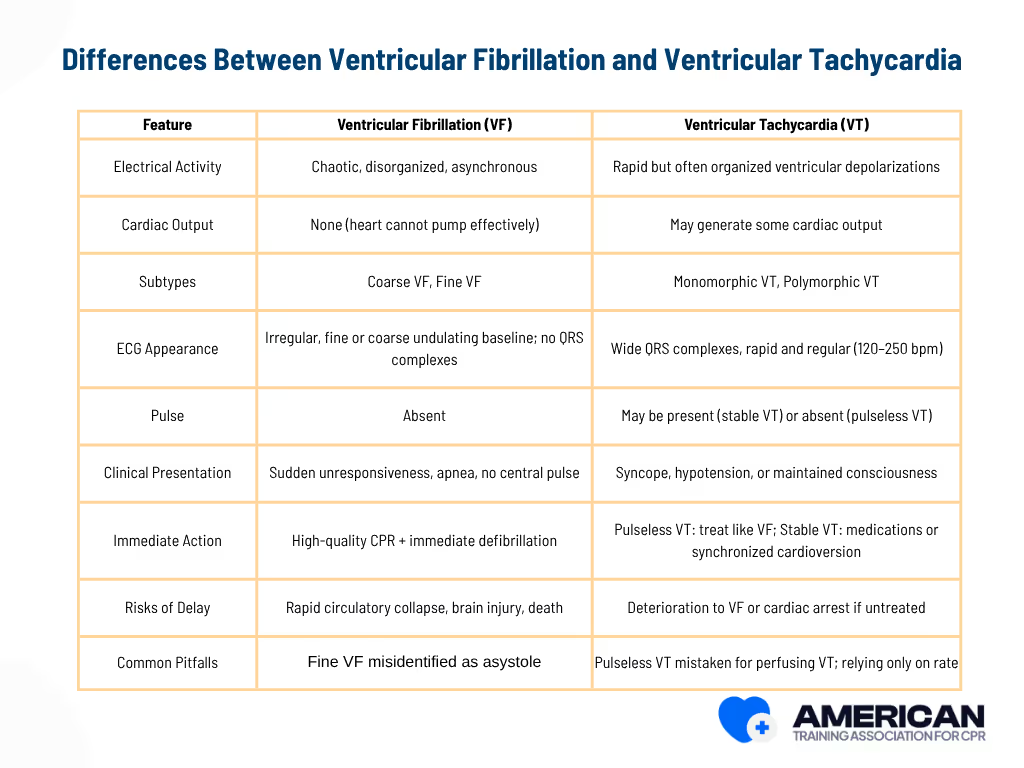
Recognizing these key differences helps rescuers prioritize defibrillation and chest compressions correctly. Proper identification of VF and VT is critical to improving survival and patient outcomes during cardiac emergencies.
What are the Causes of Ventricular Fibrillation
Ventricular fibrillation (VF) can be triggered by multiple conditions that destabilize the heart’s electrical activity. Key causal categories include acute ischemic events, structural heart disease, inherited electrical disorders, metabolic disturbances, drug toxicity, mechanical trauma, and systemic illnesses.
Common causes of VF include:
- Structural Heart Disease – Scar tissue, dilated ventricles, or valvular problems create abnormal conduction pathways that can trigger VF. Examples: post-infarction scar, dilated cardiomyopathy, hypertrophic cardiomyopathy.
- Acute Myocardial Infarction (MI) – Sudden coronary blockage causes ischemia and electrical instability, often leading to VF within minutes to hours. VF complicates 3–10% of STEMI cases.
- Chronic Ischemia / Coronary Artery Disease – Ongoing oxygen supply–demand mismatch and fibrosis increase long-term VF risk.
- Inherited Electrical Disorders / Channelopathies – Gene variants or drug-induced ion channel dysfunction can provoke life-threatening arrhythmias. Examples: long QT syndrome, Brugada syndrome, catecholaminergic polymorphic VT.
- Electrolyte Imbalances & Metabolic Disturbances – Abnormal potassium, magnesium, calcium, severe acid-base disorders, or hyperglycemia disrupt cardiac conduction and may trigger VF.
- Drug Toxicity / Medication Effects – Certain antiarrhythmics, psychotropics, stimulants, or overdoses prolong repolarization or increase sympathetic activity, provoking VF.
- Mechanical Trauma / Acute Injury – Blunt chest impact, penetrating wounds, or electrical injury can directly cause VF. Examples: commotio cordis, traumatic cardiac injury.
- Primary Electrical Events / Sudden Cardiac Triggers – Idiopathic VF or unexplained electrical storms can occur without structural heart disease, often triggered by premature ventricular complexes or Purkinje system activity.
- Systemic Conditions – Severe hypoxia, sepsis, or massive pulmonary embolism impair myocardial perfusion and can precipitate VF.
Understanding these causes helps rescuers identify high-risk situations and prioritize rapid recognition and immediate action.
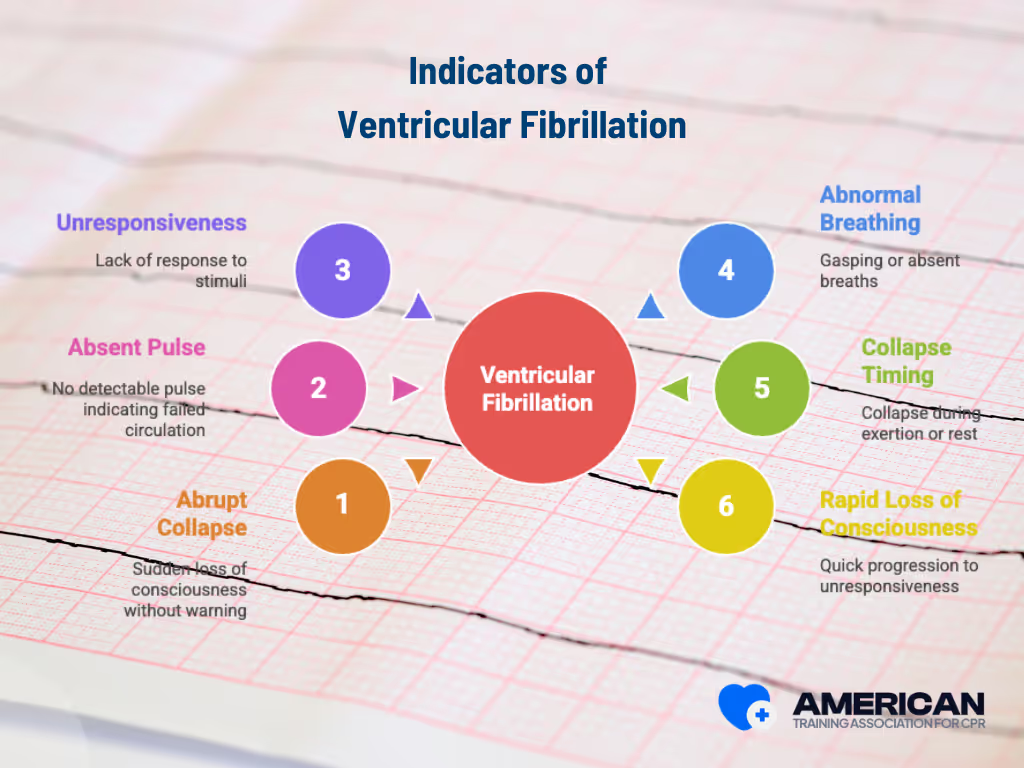
Signs and Symptoms of Ventricular Fibrillation
The primary signs of ventricular fibrillation (VF) are sudden collapse, absence of a central pulse, and global unresponsiveness. Recognizing these cues quickly is critical for initiating life-saving interventions.
Key observable signs include:
- Abrupt Collapse – Sudden loss of consciousness without warning, reflecting immediate cessation of effective cardiac output.
- Absent Pulse – No detectable carotid or femoral pulse within 5–10 seconds, indicating failed forward circulation.
- Unresponsiveness – Lack of response to verbal or physical stimuli, signaling inadequate cerebral perfusion.
- Abnormal Breathing / Agonal Respirations – Gasping or absent breaths, which are ineffective and should prompt immediate CPR.
- Collapse During Exertion or at Rest – Timing of collapse can suggest a primary cardiac rhythm disturbance, especially in adults with known heart disease.
- Rapid Loss of Consciousness – Quick progression from brief fainting to prolonged unresponsiveness distinguishes VF from reflex syncope.
The triad of abrupt collapse, absent pulse, and unresponsiveness forms the most critical bedside indicators of VF. These observable signs should prompt urgent resuscitation while preparing for confirmatory rhythm analysis, discussed in the Ventricular Fibrillation ECG section.
CPR and FIRST AID
Certification





What Does Ventricular Fibrillation Look Like on ECG?
The ECG of ventricular fibrillation (VF) shows irregular, chaotic electrical activity with no identifiable QRS complexes, indicating loss of coordinated ventricular contraction and negligible cardiac output. Immediate recognition is critical for urgent resuscitation.
Waveform Features of Ventricular Fibrillation:
- Amplitude: Coarse VF >3 mm; fine VF <3 mm (peak-to-trough on standard ECG calibration).
- Frequency: 150–500 fibrillatory waves per minute; coarse VF often slower, fine VF faster.
- Irregularity: No repeating morphology; differentiates VF from organized tachyarrhythmias.
- Absence of P waves and QRS complexes: No discrete atrial or ventricular complexes, reflecting loss of coordinated contraction.
Chaotic reentrant wavelets or disorganized ventricular activation fronts fragment normal depolarization, preventing effective mechanical contraction. The result is electrical desynchronization and minimal cardiac output.
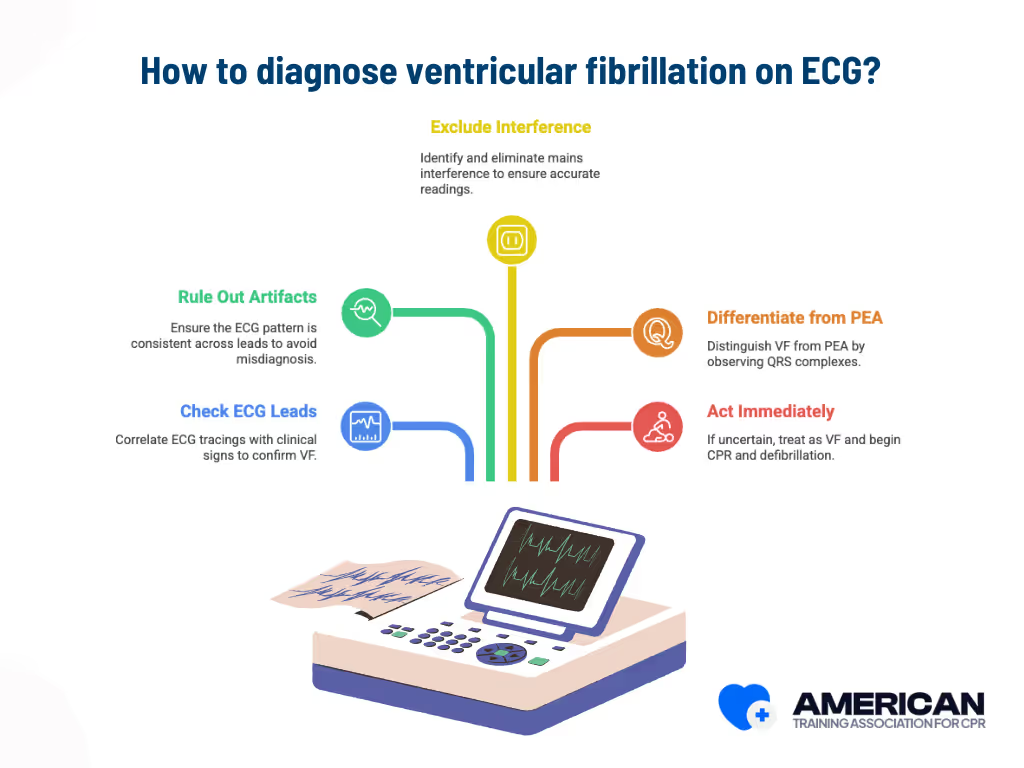
How Is Ventricular Fibrillation Diagnosed on ECG?
To confirm ventricular fibrillation (VF) on an ECG:
- Check multiple ECG leads (I, II, V1) and correlate the tracing with clinical signs such as absent pulse and unresponsiveness.
- Rule out motion artifact by noting that artifacts vary in morphology across leads, while true VF appears chaotic and consistent in all leads.
- Exclude mains interference, which has a fixed 50/60 Hz frequency and narrowband pattern.
- Differentiate VF from pulseless electrical activity (PEA): PEA shows organized QRS complexes, while VF displays a continuous chaotic baseline.
- When uncertain, act immediately: If a patient is unresponsive and pulseless with a rhythm resembling VF, treat it as VF and begin CPR and defibrillation without delay.
Recognizing VF’s ECG pattern, including its irregular amplitude, chaotic waveform, and absence of QRS complexes, is vital for immediate defibrillation and survival. The next section explains how ECG recognition guides emergency resuscitation steps.
Why Ventricular Fibrillation Is a Life Threatening Emergency
Ventricular fibrillation is a life threatening emergency because it causes a sudden loss of effective ventricular pumping, leading to the rapid stop of blood circulation and requiring immediate medical intervention.
Time is critical. Within 4 to 6 minutes, brain cells begin to suffer irreversible damage, and the heart muscle becomes less responsive to defibrillation as ischemia progresses. Without prompt action, the result is rapid loss of consciousness, organ ischemia, and eventual cardiac arrest.
Immediate cardiopulmonary resuscitation (CPR) and defibrillation are essential to restore circulation. High-quality chest compressions help maintain blood flow until a defibrillator is available. Early unsynchronized shocks remain the most effective way to end ventricular fibrillation.
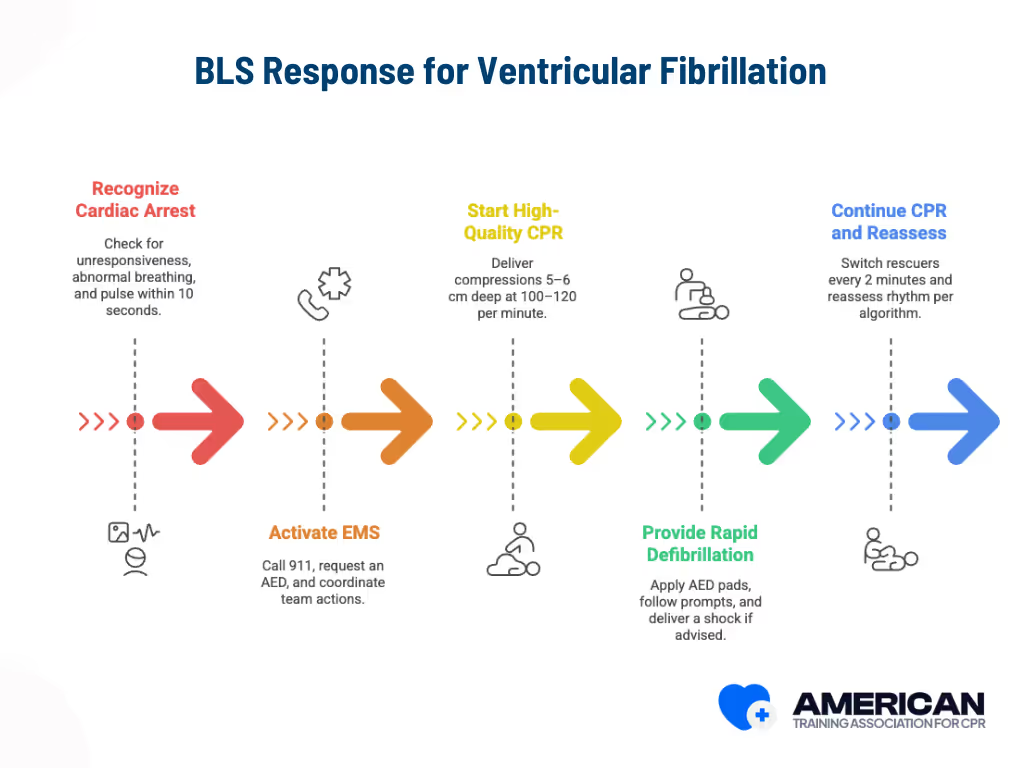
BLS Steps for Ventricular Fibrillation
The BLS response for ventricular fibrillation follows five key steps:
- Recognize cardiac arrest: Check for unresponsiveness, abnormal breathing, and pulse within 10 seconds to begin CPR quickly.
- Activate EMS: Call 911, request an AED, and coordinate team actions for timely advanced care.
- Start high-quality CPR: Deliver compressions 5–6 cm deep at 100–120 per minute with minimal interruptions and correct ventilation ratios.
- Provide rapid defibrillation: Apply AED pads, follow prompts, deliver a shock if advised, and resume CPR immediately.
- Continue CPR and reassess: Switch rescuers every 2 minutes, reassess rhythm per algorithm, and maintain perfusion until advanced help arrives.
This structured sequence minimizes delays, maximizes perfusion, and improves survival chances in ventricular fibrillation.
1. Recognize the cardiac arrest
Check for unresponsiveness and abnormal or absent breathing. Begin basic life support immediately if there is no normal breathing or only gasping. Check the carotid pulse only if trained and within 10 seconds. Quick recognition shortens the delay to CPR and AED use.
2. Call emergency medical services immediately.
Activate the emergency response system by calling 911 or directing someone to do so while requesting an AED and advanced life support. If alone and no AED is nearby, perform 2 minutes of CPR before leaving to call EMS and get the AED, if recommended locally. BLS training emphasizes role assignment and clear communication to coordinate ongoing CPR until professionals arrive.
3. Start high-quality cardiopulmonary resuscitation.
Perform chest compressions 5–6 cm deep at 100–120 per minute with full chest recoil and minimal pauses. Provide 30 compressions and 2 ventilations if a single rescuer; if an advanced airway is in place, continue compressions with 1 ventilation every 6–8 seconds. Continuous compressions maintain blood flow and improve shock success.
4. Rapid defibrillation
Apply AED pads in the correct positions: one below the right clavicle and the other on the left lateral chest. Follow AED prompts, allow rhythm analysis, and deliver a shock immediately if ventricular fibrillation is detected. Resume compressions without delay. Ensure no one touches the patient during analysis or shock. ATAC's BLS training covers AED use, safe shock procedures, and minimizing pauses.
5. Continue CPR following the BLS algorithm.
Resume compressions after each shock or when no shock is advised. Reassess rhythm and pulse every 2 minutes or as prompted by the AED. Switch rescuers every 2 minutes to limit fatigue. Continue until EMS or advanced cardiac life support teams take over. Maintaining organ perfusion between shocks increases the chance of return of spontaneous circulation. BLS training also covers timing, team roles, and use of real-time feedback devices.
What Is the ACLS Protocol for Ventricular Fibrillation?
The ACLS protocol for ventricular fibrillation aims to stop chaotic ventricular activity and restore an organized, perfusing rhythm. It prioritizes rapid rhythm recognition, immediate defibrillation, high-quality chest compressions (hands-only or compression-only CPR), and coordinated advanced interventions.
Which Medications Are Used in the ACLS Protocol for VF?
Pharmacologic therapy supports rhythm control and stabilizes hemodynamics when shocks and compressions are not enough.
Key drugs include:
- Epinephrine 1 mg IV/IO every 3–5 minutes
- Amiodarone 300 mg IV bolus, followed by 150 mg if VF persists
Adjunctive care includes vasoactive medications (norepinephrine, vasopressin), airway management, and advanced monitoring. These interventions enhance myocardial perfusion and reduce recurrence risk.
How Does BLS Certification Prepare You for Ventricular Fibrillation Emergencies?
BLS certification equips responders to recognize ventricular fibrillation (VF), perform high-quality CPR, and operate an automated external defibrillator (AED). These skills enable immediate lifesaving action that bridges the gap between cardiac arrest recognition and advanced cardiac life support.
BLS certification builds teamwork through role assignment and closed-loop communication. Trainees learn to delegate and rotate tasks, including:
- Compressor role
- Airway manager
- AED operator
Regular role briefings every 2 minutes help teams maintain focus, reduce pauses in compressions, and deliver faster defibrillation during VF scenarios. This coordination reduces confusion and enhances response efficiency under pressure.
CPR and FIRST AID
Certification





How Does BLS Certification Support the Chain of Survival?
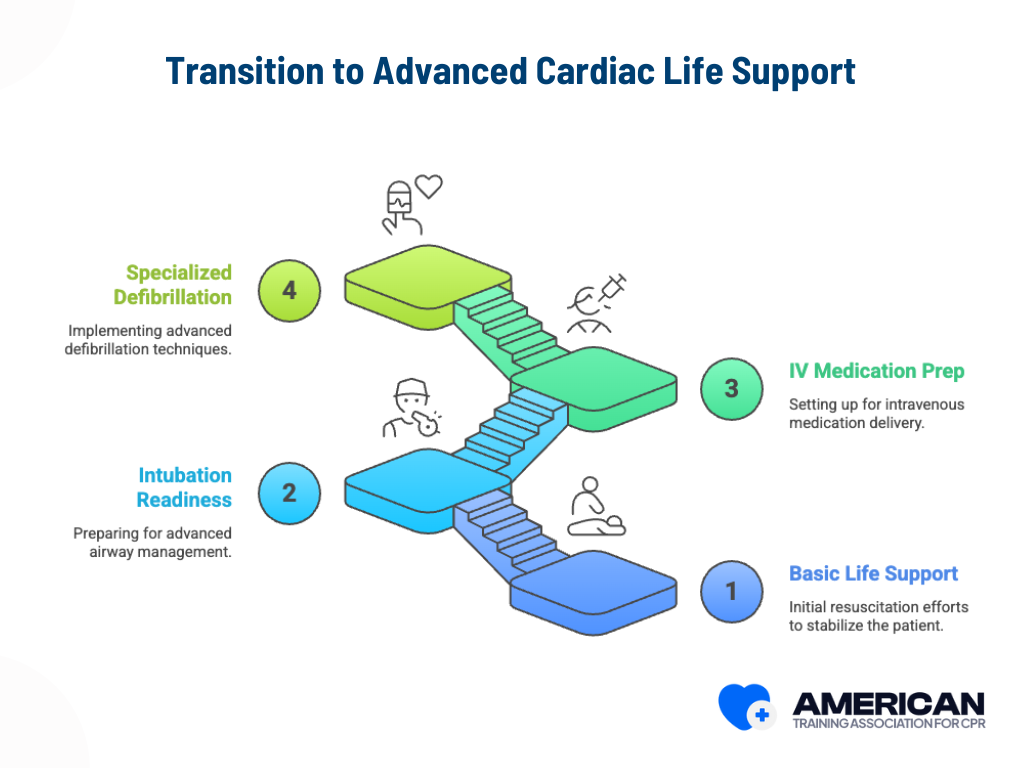
While BLS focuses on the early, critical steps of resuscitation, it also prepares responders for smooth transition to Advanced Cardiac Life Support (ACLS).
This includes readiness for advanced procedures like intubation, IV medication administration, and specialized defibrillation strategies.
Organizations such as hospitals, workplace safety programs, and online providers like ATAC’s Online BLS Certification offer comprehensive training that develops these lifesaving skills.
Unlike traditional in-person classes, ATAC’s online format allows learners to:
- Study at their own pace from any location
- Review interactive materials and videos that reinforce BLS techniques
- Earn certification quickly and conveniently without scheduling conflicts
ATAC’s online program makes high-quality, evidence-based BLS training accessible to both healthcare professionals and non-medical responders, ensuring more people are prepared to act confidently in cardiac emergencies.
Can lay rescuers use an AED for VF?
Yes. AEDs are designed for anyone to use. Follow the device’s voice prompts, attach pads correctly, clear the patient before shocking, and resume CPR immediately after the shock or if no shock is advised.
How is ventricular fibrillation related to a heart attack?
A heart attack (myocardial infarction) can trigger ventricular fibrillation by damaging the heart’s electrical system and interrupting blood flow. Quick emergency care and defibrillation are critical to restore normal rhythm and prevent heart failure.
How do doctors confirm VF or other arrhythmias?
Diagnosis involves ECG analysis, Holter monitoring, event recorders, or loop recorders to detect irregular electrical impulses. In some cases, cardiac MRI, coronary CT angiography, or electrophysiology studies are used to identify structural or electrophysiologic disorders.
What are other cardiac arrhythmias linked to VF?
Other common cardiac arrhythmias include Atrial Fibrillation, Atrial Flutter, and sinus node dysfunction. These conditions involve abnormal electrical signaling in the heart chambers, sometimes progressing to VF if untreated.
What role does an Implantable Cardioverter-Defibrillator (ICD) play?
An Implantable Cardioverter-Defibrillator automatically detects life-threatening rhythms like VF or ventricular tachycardia and delivers a life-saving shock. ICD therapy prevents sudden cardiac death in patients with heart failure, prior cardiac arrest, or inherited primary arrhythmia syndromes.
Are there treatments for recurrent VF or other arrhythmias?
Yes. Catheter ablation targets abnormal areas in the heart that cause irregular electrical impulses. Patients may also receive sodium channel blockers or cardiac resynchronization therapy for rhythm control.
Can lifestyle or health conditions increase VF risk?
Yes. Conditions such as heart failure, obstructive sleep apnea, potassium imbalances, and thyroid disorders can disrupt the heart’s electrical activity. Managing these underlying issues and maintaining healthy potassium levels help prevent arrhythmias.
How are inherited or congenital disorders linked to VF?
Some inherited primary arrhythmia syndromes and congenital disorders affect the sinoatrial node (SA node) and electrical conduction pathways. Genetic screening, multigene panels, and familial counseling help identify individuals at higher risk.
How can doctors monitor the heart’s electrical activity over time?
Tools such as a Holter monitor, event monitor, or loop recorder track the heart rhythm continuously. Exercise stress tests, tilt table tests, or epinephrine tests may also evaluate abnormal rhythm responses or exercise-induced VF.
CPR and FIRST AID
Certification





Real Stories from Our BLS Certified Participants













