It is H2 heading of the page.
It is H3 heading of the page.
It is H4 heading of the page
A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
- hello this is the list of page
- hello this is the list of page
Here is another list:
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page
- hello this is ordered list of the page

Pulseless Ventricular Tachycardia: Causes, Symptoms & BLS Response
Ventricular tachycardia is a heart rhythm disorder that originates in the lower heart chambers. It can be monomorphic VT (uniform QRS morphology) or polymorphic VT (variable shapes), and when sustained, it often leads to hemodynamic compromise or even sudden cardiac death.
Early basic life support (BLS), including high-quality CPR and rapid defibrillation, improves outcomes by restoring perfusion and buying time for advanced care. Without immediate action, survival chances drop within minutes. Understanding this rhythm, why it happens, and what to do is essential for both healthcare providers and trained rescuers.
What is Pulseless Ventricular Tachycardia?
Pulseless ventricular tachycardia produces zero effective cardiac output (no pulse), making it a form of cardiac arrest that requires prompt defibrillation. Rapid ventricular rates shorten diastolic filling time, drastically reducing stroke volume and cardiac output, resulting in pulseless ventricular tachycardia. VT usually shows QRS complexes >120 ms with minimal beat-to-beat variation, forming a wide-complex, regular rhythm on ECG.
In a pulseless patient, it should be treated immediately as a shockable cardiac arrest rhythm. The ventricles contract too fast and inefficiently, preventing enough stroke volume to generate a pulse and leading directly to circulatory collapse.
Pulseless VT differs from ventricular fibrillation (VF). VT shows organized, repetitive ventricular complexes with uniform morphology, while VF appears as chaotic, low-amplitude waves without QRS complexes. This organized pattern in pulseless VT makes it recognizable on a monitor and explains why it is considered a shockable rhythm.
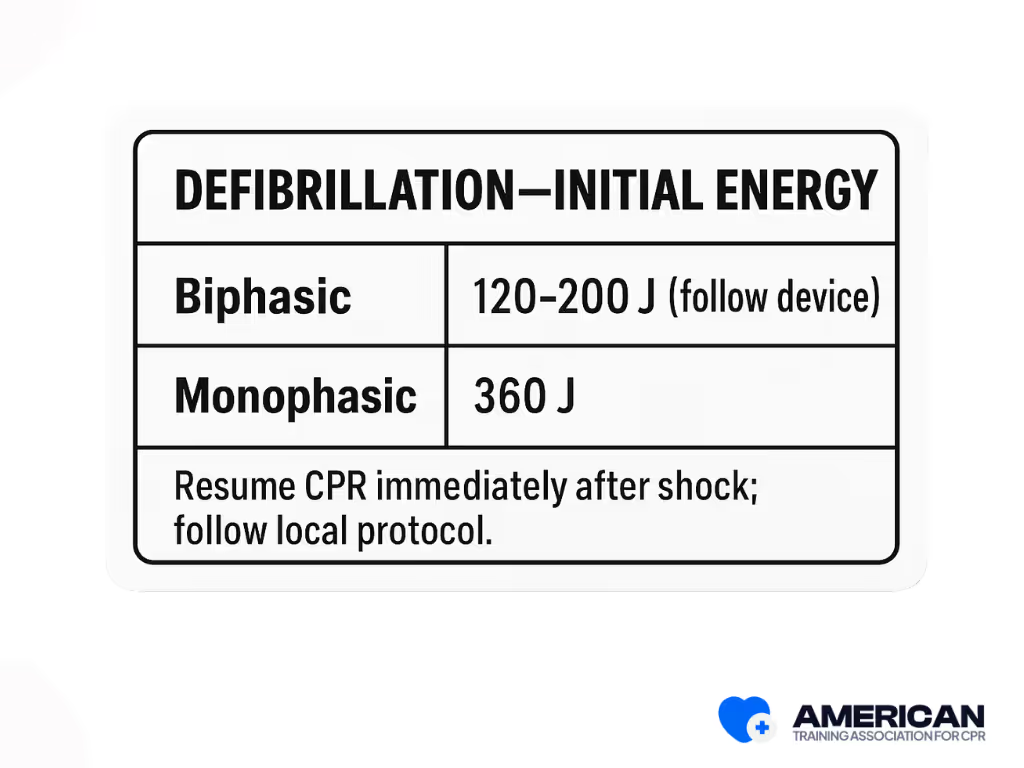
Defibrillation works by delivering a strong electrical shock that depolarizes the ventricles, interrupting the circuits that sustain VT. Deliver one shock using the device-recommended energy setting (typically 120–200 J for biphasic defibrillators; 360 J for monophasic). Immediately resume CPR.
Because pulseless VT equals cardiac arrest, urgent measures are needed:
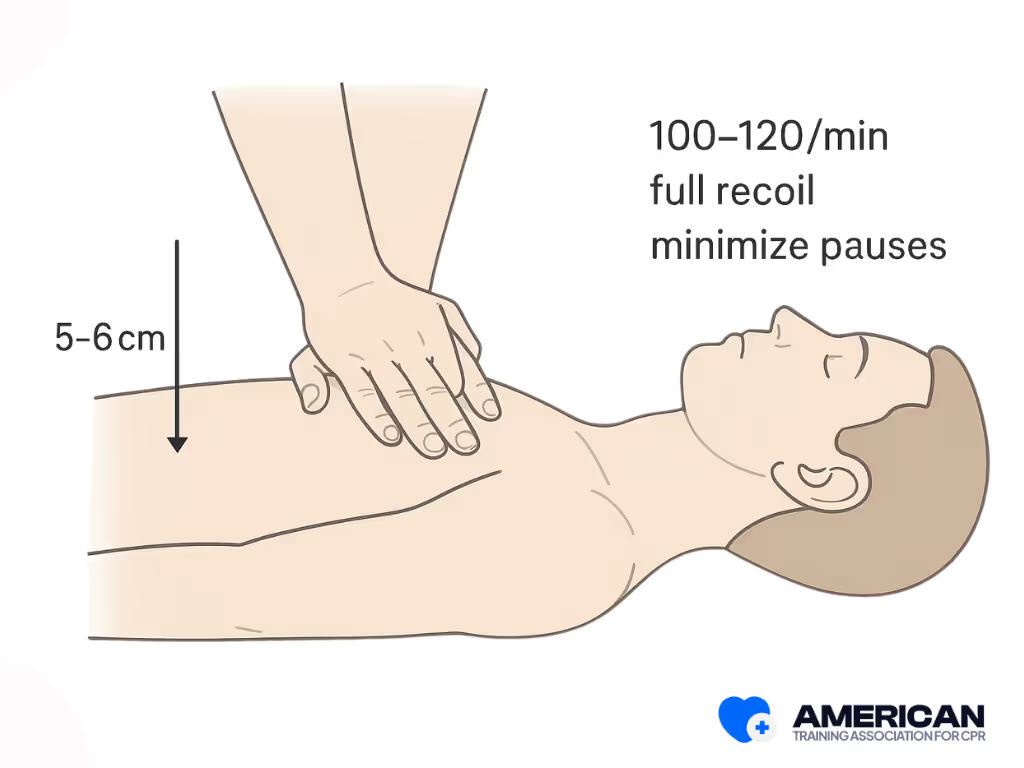
- Chest compressions: 100–120 per minute, at 5–6 cm (approx. 2–2.4 inches) deep in adults, based on current BLS guideline standards.
- Prompt defibrillation when the rhythm is identified.
- Airway and breathing support as needed.
How is pulseless VT different from ventricular fibrillation?
Pulseless VT shows a rapid, wide, organized rhythm, while VF looks chaotic and irregular. Both require CPR and defibrillation, but recognition helps guide care.
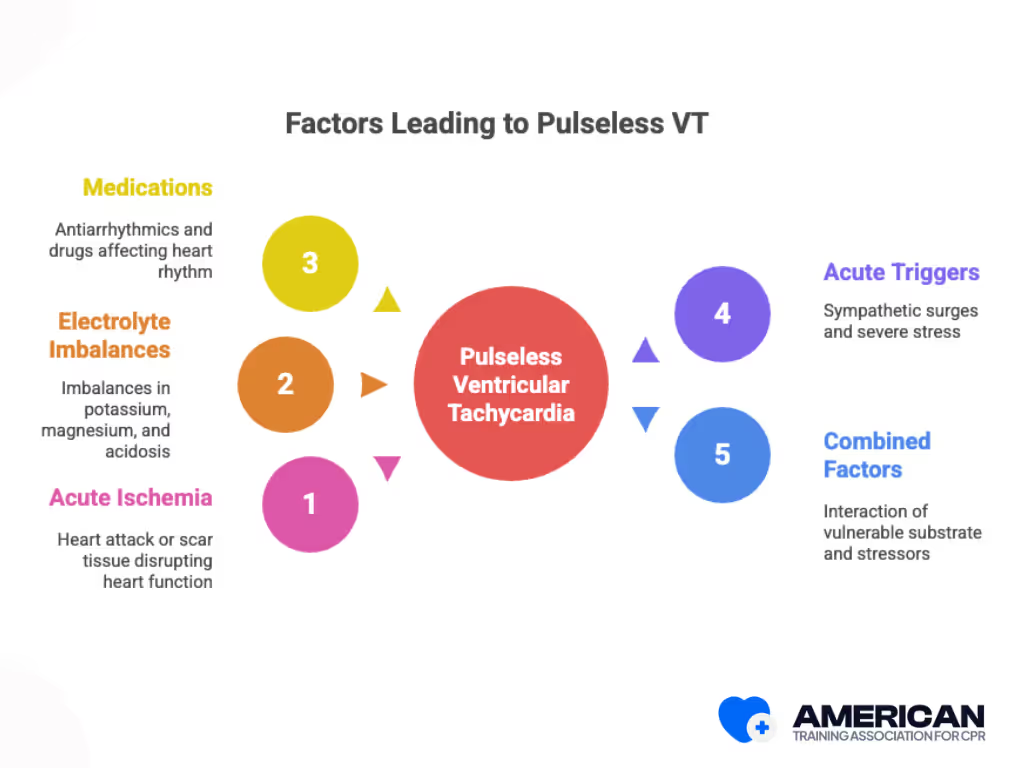
What Causes Pulseless Ventricular Tachycardia?
Pulseless Ventricular Tachycardia (VT) develops from several disturbances that disrupt normal heart conduction:
- Acute ischemia and structural heart disease: Heart attack, scar tissue, or cardiomyopathy creating reentry circuits.
- Electrolyte and metabolic imbalances: Hypokalemia, hyperkalemia, hypomagnesemia, and severe acidosis.
- Medications and medical factors: Antiarrhythmics, drugs prolonging repolarization, electrolyte shifts, reperfusion injury, and device malfunctions.
- Acute triggers: Sympathetic surges, blood loss, respiratory failure, or severe stress.
- Combined factors: Interaction of a vulnerable substrate (scarred myocardium), acute trigger (ischemia, electrolyte disturbance), and stressor (hypoxia, acidosis).
Because these factors often overlap, fast recognition and treatment are crucial to survival.
How do electrolyte imbalances specifically increase the risk of pulseless ventricular tachycardia?
Electrolytes regulate the heart’s electrical activity. Low potassium (hypokalemia) delays repolarization, making the heart excitable. High potassium (hyperkalemia) slows conduction, while low magnesium (hypomagnesemia) can trigger torsades de pointes. These shifts destabilize electrical signaling, increasing VT risk.
Why is pulseless ventricular tachycardia considered more dangerous than other arrhythmias?
Unlike cardiac arrhythmias where some circulation remains, pulseless VT immediately stops effective blood flow. This causes rapid organ failure and brain injury within minutes, making it a true cardiac arrest rhythm that requires urgent defibrillation and CPR.
How can Basic Life Support (BLS) training help respond effectively to pulseless VT?
BLS training teaches recognition of cardiac arrest, how to start chest compressions immediately, and how to use an AED for defibrillation. These quick actions double or triple survival chances before professional care arrives.
CPR and FIRST AID
Certification





What are the Signs and Symptoms of Pulseless VT?
Pulseless Ventricular Tachycardia (VT) presents with sudden collapse, unresponsiveness, absent central pulse, and abnormal or absent breathing. These signs should trigger immediate Basic Life Support and activation of emergency medical services.
- Sudden collapse and unresponsiveness: Loss of posture and consciousness signal abrupt cessation of circulation. If witnessed, bystanders should call for help and begin chest compressions within 10 seconds if there is no normal breathing.
- Absent pulse and abnormal breathing: A missing carotid or femoral pulse (checked for no more than 10 seconds) and absent or irregular respirations confirm cardiac arrest. An AED should be attached as soon as possible, with compressions paused only briefly.
- Peripheral signs: Skin pallor, cyanosis, sweating, dilated pupils, and lack of response may support the diagnosis but must not delay CPR or defibrillation.
What Does Pulseless Ventricular Tachycardia Look Like on an ECG?
On an ECG, pulseless ventricular tachycardia (VT) appears as a rapid ventricular rhythm with wide, uniform QRS complexes and a regular pattern. Although electrically organized, the rhythm produces no effective cardiac output, making it a cardiac arrest emergency.
Key ECG features:
- Sustained wide QRS complexes (>120 ms), often resembling bundle branch block or pacing patterns.
- Ventricular rate typically 100–250 beats per minute.
- Absence of P waves or consistent PR intervals.
- Regular R-to-R intervals, usually monomorphic in appearance.
Why wide QRS matters?
A wide QRS indicates a ventricular origin of the rhythm. While bundle branch block or preexisting conduction disease can also produce wide complexes, in the context of collapse and no pulse, it supports the diagnosis of pulseless VT.
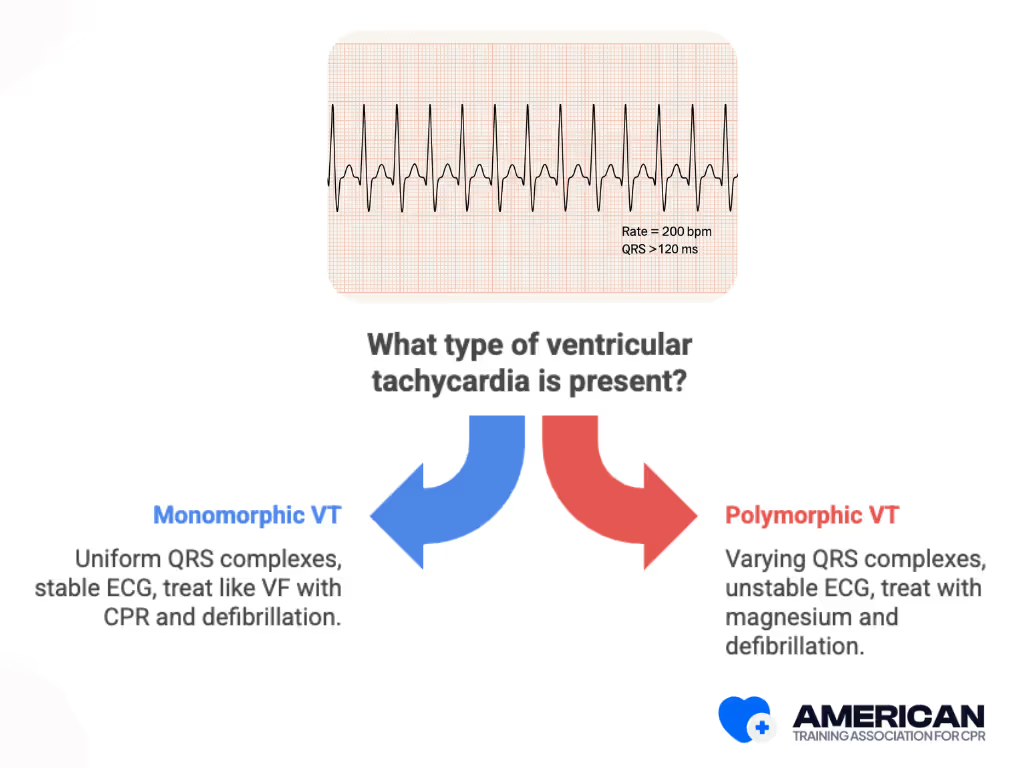
What Is the Difference Between Monomorphic and Polymorphic VT?
Ventricular tachycardia (VT) can appear in two main forms, which affect how it looks on the ECG and sometimes how it is managed:
- Monomorphic Ventricular Tachycardia: QRS complexes look uniform, often due to scar tissue; more stable on ECG; if pulseless, treat like VF with CPR and defibrillation.
- Polymorphic Ventricular tachycardia: QRS complexes vary in shape/size; linked to ischemia, electrolyte imbalance, or prolonged QT; less stable, can turn into VF.
Both can be fatal when pulseless. Immediate CPR and defibrillation are essential. Magnesium sulfate is used in cases of torsades de pointes (a specific form of polymorphic VT associated with prolonged QT). This is an advanced life support (ALS) intervention.
Why Is Pulseless Ventricular Tachycardia a Life-Threatening Emergency?
Pulseless ventricular tachycardia (VT) is a cardiovascular emergency because it abolishes effective cardiac output, cutting off oxygenated blood flow to the brain, heart, and vital organs. Without rapid CPR and defibrillation, it progresses within minutes to irreversible organ injury and death.
- Mechanism of collapse: With no effective ventricular contraction, stroke volume drops to zero, halting aortic outflow, pulmonary circulation, and coronary perfusion. Oxygen delivery stops, cells switch to anaerobic metabolism, and energy failure accelerates myocardial instability and neuronal necrosis.
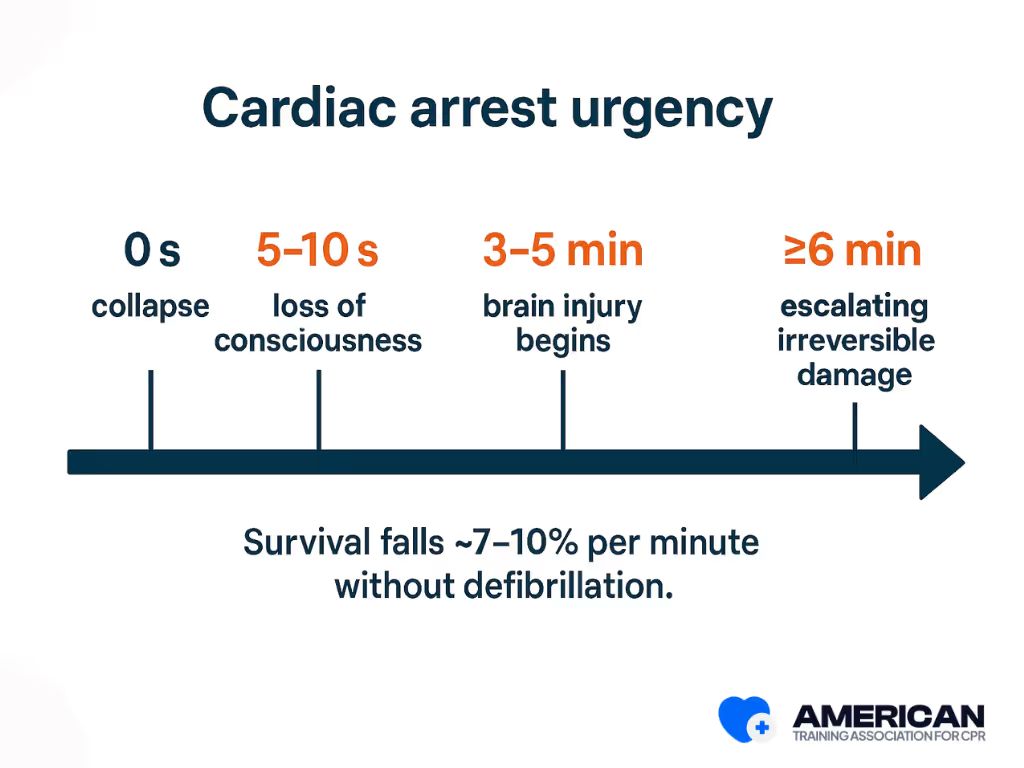
- Critical time window: Loss of consciousness occurs in 5–10 seconds, severe brain injury begins around 3–5 minutes, and irreversible neuronal damage escalates after 6 minutes without oxygen. Myocardial ischemia and worsening arrhythmia occur in the same timeframe, underscoring the need for immediate reversal.
- Immediate risks: Pulseless VT often degenerates into ventricular fibrillation, worsening electrical chaos. Survival may decrease by approximately 7–10% per minute without defibrillation, though this varies by response time and bystander CPR.
- Life-saving interventions: High-quality CPR provides limited but vital coronary and cerebral perfusion. Rapid defibrillation interrupts the arrhythmia to restore organized output. Effective CPR requires 100–120 compressions per minute, depth of 5–6 cm, full recoil, and minimal pauses. Early basic life support and defibrillation remain the only proven time-sensitive measures that can restore life.
- Impact of delay: Every minute without CPR and shock worsens outcomes, reducing survival and increasing neurologic injury. Even with advanced care, delayed recognition leads to poor hospital discharge survival and high rates of permanent impairment.
Pulseless VT is life-threatening because it produces immediate circulatory arrest. Only prompt CPR and defibrillation can restore perfusion and prevent irreversible organ damage.
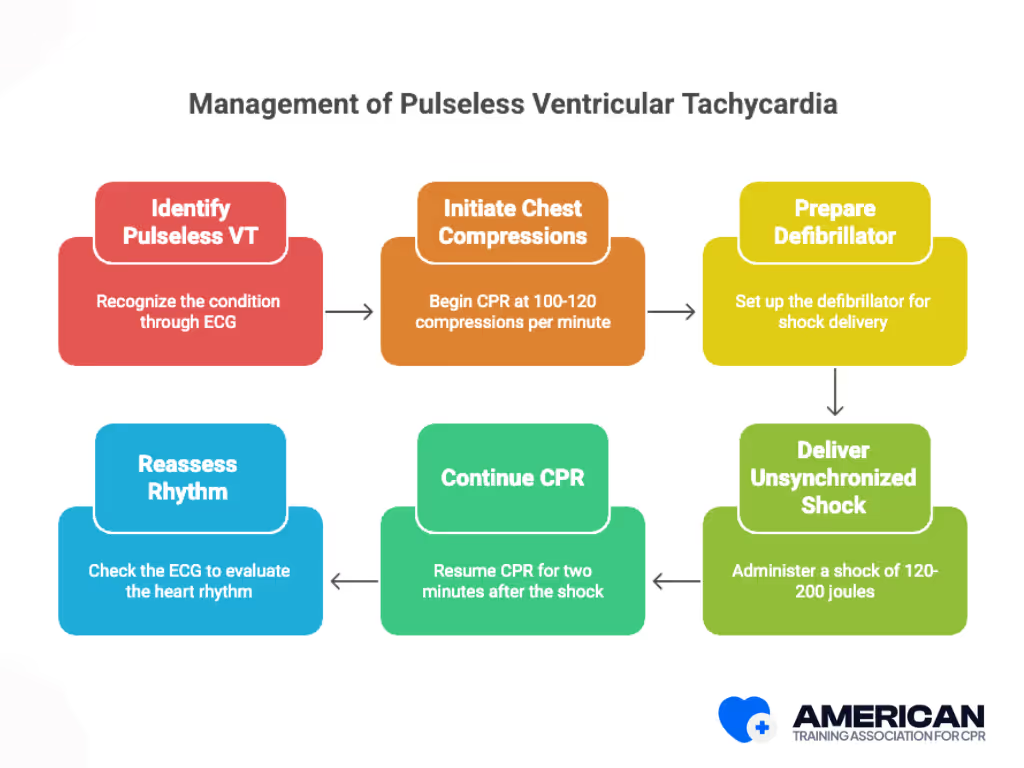
What Are the BLS Steps for Pulseless Ventricular Tachycardia?
When encountering pulseless ventricular tachycardia, rescuers must follow a structured sequence of basic life support actions. The goal is to maintain circulation and deliver defibrillation as quickly as possible. These steps apply to both lay rescuers and first responders, with timing, coordination, and safety integrated throughout.
- Check Responsiveness and Breathing: Identify unresponsiveness, absent normal breathing, and lack of a carotid pulse within 10 seconds. Quickly assess while assigning another bystander to call emergency services.
- Activate Emergency Services: Call for help immediately and request an AED. If alone with a mobile phone, dial the 911 on speaker while beginning CPR.
- Begin High-Quality CPR: Perform chest compressions at a rate of 100–120 per minute and a depth of 5–6 cm (2–2.4 inches) in adults, allowing full chest recoil. Keep hands on the lower half of the sternum and minimize pauses. Switch compressors every 2 minutes to avoid fatigue.
- Use an AED: Turn on the device, attach pads to the bare chest, and follow prompts. Ensure everyone is clear before shock delivery. Resume compressions immediately after the shock.
.avif)
What Comes After the First Defibrillation Cycle?
After the first defibrillation cycle, continue CPR and ventilation in cycles. Reassess rhythm every 2 minutes or as prompted by the AED. Persist until advanced life support arrives.
The sequence emphasizes early recognition, immediate CPR, and rapid defibrillation; the core of BLS for pulseless ventricular tachycardia. Consistently practicing these steps during training ensures confidence and effectiveness in real emergencies.
CPR and FIRST AID
Certification





What Is the ACLS Protocol for Pulseless Ventricular Tachycardia?
Pulseless ventricular tachycardia follows the same Basic Life Support (BLS) steps, starting with checking responsiveness, calling for help, and assessing breathing and pulse. The key difference is that in pulseless VT, no pulse is detected even though the heart shows electrical activity. Once identified, CPR should begin immediately with high-quality chest compressions, and attaching an AED or defibrillator becomes critical since defibrillation is usually required to restore a normal rhythm.
Unlike standard BLS, where an AED may or may not advise a shock, in pulseless VT, the defibrillator typically recommends it, making rapid shock delivery the life-saving step before resuming CPR.
Why Are Early CPR and Defibrillation Important?
Early CPR and Defibrillation are important because they keep blood and oxygen flowing when the heart stops, buying time until advanced help arrives. Defibrillation is the only way to restore a normal rhythm, and every minute without it lowers survival by 7–10%. Bystander CPR helps slow this decline, making quick action critical for survival and brain protection.
How BLS Certification Prepares You for Pulseless VT Emergencies
BLS certification prepares responders to act quickly and effectively in pulseless ventricular tachycardia by teaching essential skills, clear decision-making steps, and team coordination. These skills shorten the time to CPR and defibrillation, improve survival rates, and build the confidence to act under pressure.
- Core Skills: Learn how to recognize unresponsiveness, check for breathing and pulse within 10 seconds, perform high-quality chest compressions (2 inches deep, 100–120 per minute, full recoil), provide effective ventilations with a bag-valve mask, and operate an AED safely with correct pad placement and shock delivery.
- Decision-Making: Training emphasizes simple resuscitation algorithms (CAB/ABC) and rhythm recognition. When the AED detects a shockable rhythm, responders are taught to deliver a shock immediately and resume CPR for two minutes before rechecking.
- Teamwork: Scenarios focus on role assignments (compressor, airway manager, AED operator, recorder), closed-loop communication, and switching compressors every two minutes to maintain quality. Coordinated action reduces pauses and improves defibrillation success.
- Confidence & Legal Awareness: Courses cover Good Samaritan laws, consent, and employer reporting protocols while offering hands-on practice. This builds confidence, reduces hesitation, and helps responders act quickly during real emergencies.
- Ongoing Practice: Certification includes skills testing and recommends renewal every two years, along with regular practice drills to keep CPR quality, AED proficiency, and teamwork sharp.
- Pathway to Training: The American Training Association for CPR offers accessible online BLS certification, with structured lessons, skills checks, and recognized credentials to prepare individuals and teams for pulseless VT emergencies.
BLS certification equips responders with lifesaving skills, structured decision-making, and teamwork readiness while clarifying legal protections and the limits of care.
CPR and FIRST AID
Certification





How does VT affect the heart and circulation?
During VT, rapid abnormal electrical signals disrupt the ventricles, preventing the heart muscle from pumping blood effectively. This can lower blood pressure, reduce oxygen delivery, and cause collapse if untreated.
What conditions increase the risk of VT?
Underlying coronary artery disease, myocardial infarction, heart failure, long QT syndrome, and inherited conditions such as Brugada syndrome or catecholaminergic polymorphic VT can all trigger episodes of sustained ventricular tachycardia.
How is VT different from other arrhythmias?
Unlike sinus tachycardia (driven by the sinus node), VT comes from the ventricles. It differs from ventricular fibrillation or torsade de pointes, but all are dangerous rhythms that require urgent care.
How is VT treated?
Treatment depends on stability and recurrence. Emergency care often includes defibrillation, antiarrhythmic drugs, or cardiopulmonary resuscitation if pulseless. If ventricular tachycardia is present with a pulse and the patient is unstable, synchronized cardioversion is typically indicated. Pulseless VT is treated as cardiac arrest with immediate defibrillation. Long-term prevention may involve catheter ablation (including radiofrequency ablation), implantable cardioverter defibrillator (ICD) therapy, or beta blockers.
What procedures help diagnose VT?
Clinicians may use electrophysiology studies, Cardiac MRI, Holter monitoring, or genetic testing to identify causes. Some cases link to structural problems such as heart valve disease, myocardial scar tissue, or impaired left ventricular function.
Can VT be prevented?
Yes. Lifestyle changes, treatment of heart failure or coronary artery disease, and medications can reduce risk. Patients with high risk for sudden cardiac death may benefit from implantable defibrillators. In selected cases, catheter ablation or cardiac surgery may be required if medications fail.
What should bystanders do if someone collapses from VT?
Immediate cardiopulmonary resuscitation and rapid defibrillation are critical. Public access to defibrillation through AEDs saves lives by restoring normal electrical impulses before irreversible injury occurs. Attach an AED as soon as it becomes available and follow the device prompts without delaying chest compressions.
Real Stories from Our BLS Certified Participants













