A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
Here is another list:

The adult chain of survival is a framework that outlines lifesaving steps after sudden cardiac arrest. Its purpose is to guide timely actions that improve survival and protect brain function.
It emphasizes early recognition of cardiac arrest and bystander CPR, rapid defibrillation, EMS response, and hospital-based post-arrest care.
This framework applies to adults in out-of-hospital settings and is based on guidelines from the American Heart Association and European Resuscitation Council.
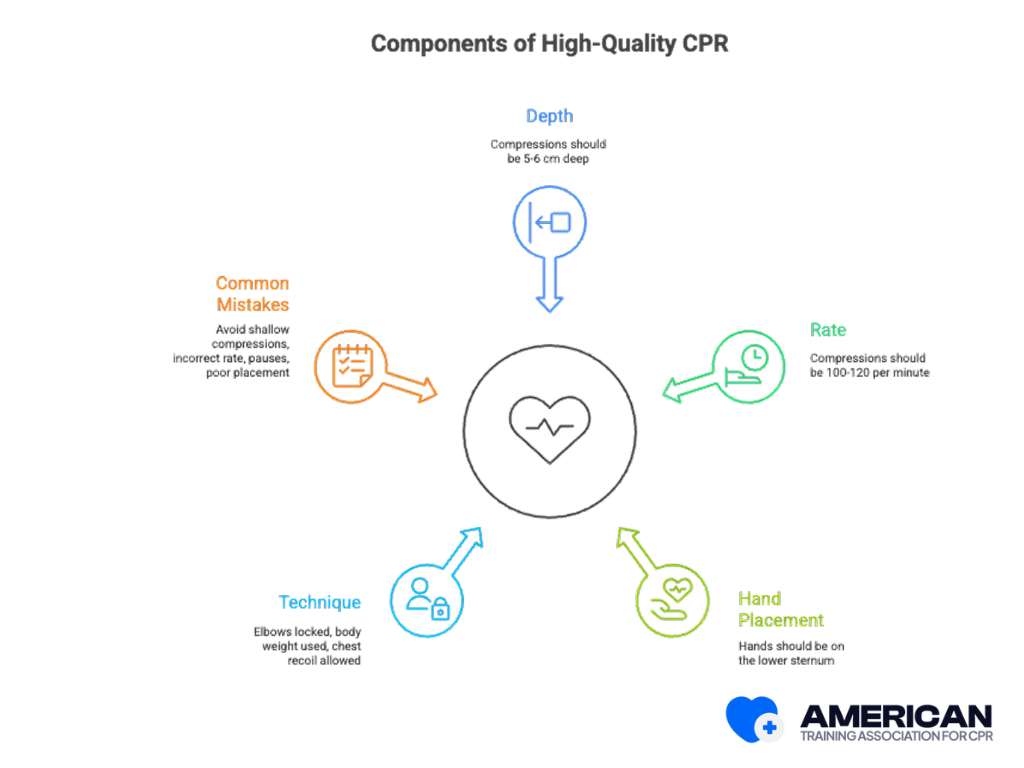
The chain is important because fast, high-quality CPR (100–120 compressions per minute, 5–6 cm depth, minimal interruptions) and rapid intervention increase survival and reduce preventable deaths. It also strengthens community readiness and reduces long-term healthcare impact.
The five links in the adult chain of survival are connected actions that work together to improve survival after out-of-hospital cardiac arrest. Each step builds on the previous one, creating a complete pathway from recognition to recovery.
Together, these five links form an integrated sequence where each step enables the next, giving the patient the best chance of survival and recovery.

This step begins when a bystander recognizes cardiac arrest and calls emergency services without delay. Early recognition shortens time to care, allows dispatcher-assisted CPR, and speeds ambulance arrival. This first step turns a sudden collapse into an active resuscitation effort.
Check for:
If unsure, treat it as cardiac arrest and call for help immediately. Many rescuers lose time double-checking breathing or pulse, which delays care. Training through a CPR course improves recognition skills and builds confidence.
Trained 911 call takers can guide you through hands-only CPR until EMS personnel arrive, improving survival rates. When activating Emergency Medical Services:
While waiting for emergency response, ensure scene safety and begin chest compressions at 100–120 per minute, 5–6 cm deep, with full recoil and minimal pauses. Continue until professionals arrive or an AED gives further instructions.
Early recognition and EMS activation shortens time to treatment, allowing CPR and defibrillation to begin quickly, the next critical link in the chain.
Once cardiac arrest is recognized, start CPR immediately, focusing on continuous, high-quality chest compressions until advanced care arrives. Perform chest compressions at 100–120 per minute, 5–6 cm deep, with minimal pauses and full chest recoil. Trained rescuers add ventilations at a 30:2 ratio; untrained rescuers can do compression-only CPR.
Why this step matters?
Chest compressions keep blood flowing to the heart and brain, buying time until defibrillation or advanced treatment can restore normal rhythm.
Team approach:
Scene safety comes first. Rib fractures can occur but are not a reason to stop. Chest compressions are lifesaving and should not be delayed.
Early, high-quality CPR preserves blood flow until the next step: rapid defibrillation.





Rapid defibrillation is the prompt delivery of an electric shock from a defibrillator to restore an effective heart rhythm. It greatly increases survival after sudden cardiac arrest.
An automated external defibrillator (AED) should be used as soon as it is available. Follow voice prompts and resume CPR immediately after shock delivery.
Sudden cardiac arrest often involves shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia. A defibrillator stops chaotic electrical activity so the heart’s natural pacemaker can restore an organized rhythm. Survival rates drop 7–10% for every minute defibrillation is delayed, so delivering a shock within 3–5 minutes is critical.

Special considerations:
Defibrillation, combined with ongoing CPR, restores normal rhythm in shockable arrests like ventricular fibrillation or pulseless ventricular tachycardia.
Advanced Life Support is provided by professional emergency responders to stabilize circulation and organ perfusion after initial resuscitation. Its role is to turn early CPR and defibrillation gains into sustained recovery through airway management, vascular access, medications, and monitoring. Core components of ALS includes:
Emergency teams work together to maintain high-quality compressions, deliver shocks promptly, and assign clear roles for compressions, airway, vascular access, monitoring, and leadership. Interventions are synchronized with compressions to reduce pauses.
Medications support circulation and rhythm stability:
Monitoring helps guide decisions. Capnography shows CPR quality—EtCO₂ under 10 mm Hg signals poor compressions, while a sudden rise suggests return of spontaneous circulation (ROSC). Providers must also decide when to secure an advanced airway, escalate circulatory support, or transport quickly if progress stalls.
After ROSC, ALS providers stabilize oxygenation (SpO₂ 94–98%), maintain blood pressure (MAP ≥65 mm Hg), and prepare for hospital interventions such as coronary angiography or temperature management.
ALS consolidates CPR and defibrillation into advanced airway, vascular, medication, and monitoring strategies. It bridges prehospital resuscitation with hospital-based post–cardiac arrest care.
After return of spontaneous circulation (ROSC), care focuses on stabilizing the patient, protecting organs, and supporting brain recovery. This step is crucial because it shapes both survival and long-term quality of life.
The first priority is to maintain blood flow and oxygen. Teams monitor the heart, blood pressure, and oxygen levels closely. Airway management, ventilator support, and vasopressors like norepinephrine help sustain circulation. Careful fluid balance and frequent neurologic checks guide treatment.
Targeted therapies improve outcomes by addressing specific needs:
Recovery also requires early rehabilitation planning. Doctors assess brain function with neurologic exams, EEG, and biomarkers. Physical and cognitive rehab may begin within 48–72 hours, while discharge planning ensures follow-up care, rehab referrals, and patient education on heart health.
Systems of care strengthen this link. Multidisciplinary hospital teams follow clear protocols, and regional cardiac arrest centers provide specialized treatment. Registries and audits track outcomes, driving continuous improvement.
Together, stabilization, targeted therapies, and rehabilitation turn ROSC into meaningful recovery and complete the Adult Chain of Survival.

The adult and pediatric chains of survival share the same goal: preventing death from cardiac arrest. However, recent updates from the American Heart Association (2025) have unified the Chain of Survival for all ages, meaning the overall steps and priorities are now consistent for adults, children, and even neonates.
Previously, differences existed due to the typical causes of arrest and patient physiology:
With the 2025 update, the unified Chain of Survival now emphasizes early recognition, high-quality CPR, rapid defibrillation, advanced life support, and integrated post-arrest care for all ages. While certain technical considerations like compression depth and weight-based medication dosing, still vary by age, the overall framework and priorities for intervention are now the same.





When cardiac arrest happens outside the hospital, survival often depends on what bystanders do in the first few minutes before EMS arrives. Calling emergency services, starting chest compressions at 100–120 per minute, and using an AED immediately can keep blood flowing and restore a shockable rhythm.
Many hesitate due to fear of legal issues, lack of training, or uncertainty about AED use. In reality, Good Samaritan laws protect rescuers, compression-only CPR is effective, and AEDs give step-by-step prompts. Quick bystander action bridges the gap until medical professionals arrive, making CPR training and certification essential.
A CPR certification course gives you the knowledge, hands-on skills, and confidence to act during cardiac arrest. It strengthens every link in the Adult Chain of Survival: recognition, CPR quality, AED use, advanced care integration, and post-arrest continuity.
Without training, many bystanders hesitate due to uncertainty, fear of causing harm, poor technique, or confusion with AEDs. Certification overcomes these barriers by teaching clear steps, providing practice, and boosting confidence.
What you learn in CPR certification:
Certification also reduces psychological barriers by clarifying Good Samaritan protections and reinforcing that quick action saves lives. While core training covers compressions, rescue breaths, and AED operation, skills can fade within a year, making regular refreshers essential.
ATAC's courses provide structured online lessons and interactive materials that build real-world readiness. Certification turns a hesitant bystander into a confident responder, ready to act when every second matters.
Enroll today in online CPR certification and be ready to save a life.





Yes. For witnessed sudden collapse in adults or teens, hands-only CPR is proven to save lives. For children, drowning, or overdose, rescue breaths are still needed
BLS covers early recognition, high-quality CPR, use of an AED, and activation of EMS personnel. It is taught by organizations like the American Heart Association and the Red Cross.
AEDs analyze heart rhythms and deliver shocks if needed. Correct electrode pad placement and minimizing peri-shock pauses are critical for patient outcomes.
Not routinely. Current AHA guidelines emphasize “temperature control” within 32–37.5 °C rather than mandatory hypothermia.
No. Immediate cath lab is required for STEMI or unstable patients. Others may not benefit from routine urgent angiography.
The Cardiac Arrest Registry to Enhance Survival collects national data linking dispatch, EMS, and hospital care to improve patient outcomes.
Not generally. They’re useful in transport or limited-staff settings but haven’t shown overall survival benefits over manual CPR.


