A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
Here is another list:

Cardiac arrest inside a hospital demands swift, coordinated action. The In‑Hospital Chain of Survival is a structured sequence designed to improve outcomes when a patient arrests within a healthcare facility. As part of the 2025 American Heart Association (AHA) updates, this chain aligns with the unified approach to cardiac arrest care, integrating prevention, recognition, intervention, and recovery under one framework. By understanding each link, every hospital team member plays a vital role in saving lives and preserving brain function.
The key links in this unified Chain of Survival remain:
This unified approach ensures clarity, consistency, and better outcomes across all cardiac arrest situations.
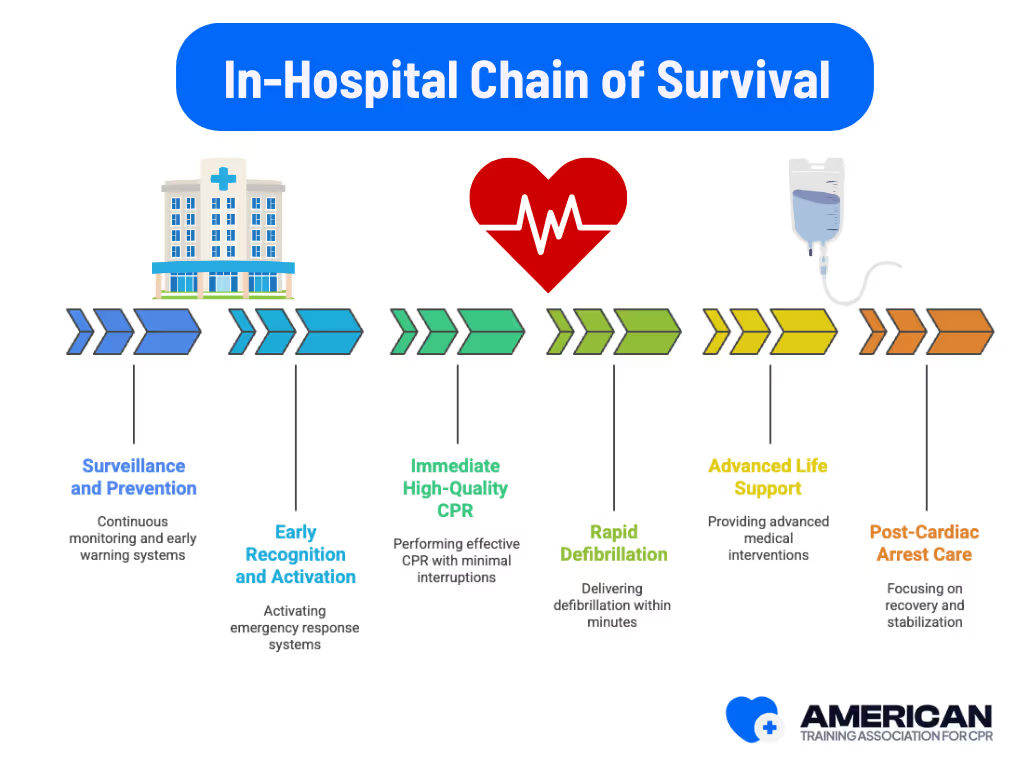





The In-Hospital Chain of Survival is not six separate tasks, but a connected system. Effective surveillance prevents many arrests before they happen. When cardiac arrest does occur, rapid recognition and activation trigger immediate CPR and defibrillation. These time sensitive actions sustain vital organs until advanced life support can be delivered. Finally, post–cardiac arrest care gives patients the best chance of meaningful recovery. Hospitals that carry out all six links in sequence significantly improve survival and neurological outcomes.
ATAC’s online CPR certification equips healthcare workers and non-medical staff with the knowledge and confidence to perform these lifesaving actions. By understanding each part of the chain, trainees can appreciate how their role fits into the bigger picture of saving lives inside a hospital.
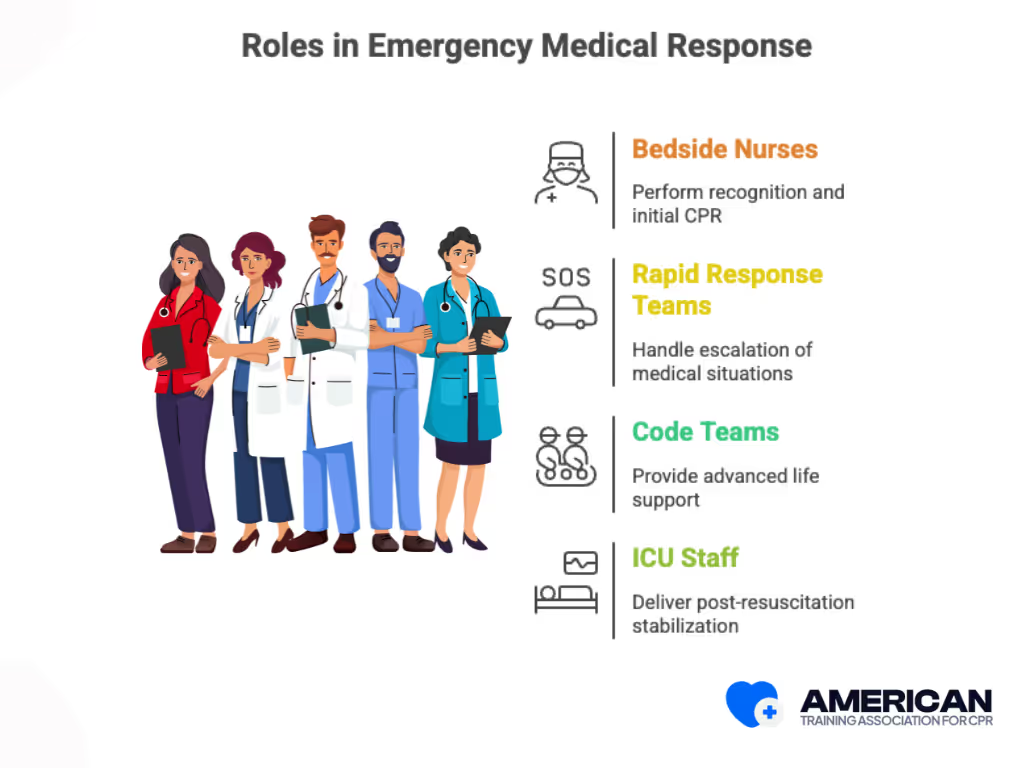
Bedside nurses, rapid response teams, code teams led by physicians or advanced practice providers, respiratory therapists, and ICU staff. Typical locations include wards, emergency departments, ICUs, and procedural suites. Nurses often perform recognition and initial CPR, response teams handle escalation, code teams provide advanced life support, and ICU teams deliver post-resuscitation stabilization.
The chain’s benefits come from speed, coordination, and skill. Faster recognition and activation shorten no-flow time, while high-quality compressions and early defibrillation improve circulation. Coordinated post-resuscitation care preserves organ function. For example, providing chest compressions immediately and defibrillation within minutes for ventricular fibrillation is linked to higher survival to discharge.
The In-Hospital Chain of Survival complements related frameworks such as the out-of-hospital chain used by EMS and rapid response systems. Some hospitals adapt it for pediatric wards or specialized areas like catheterization labs.
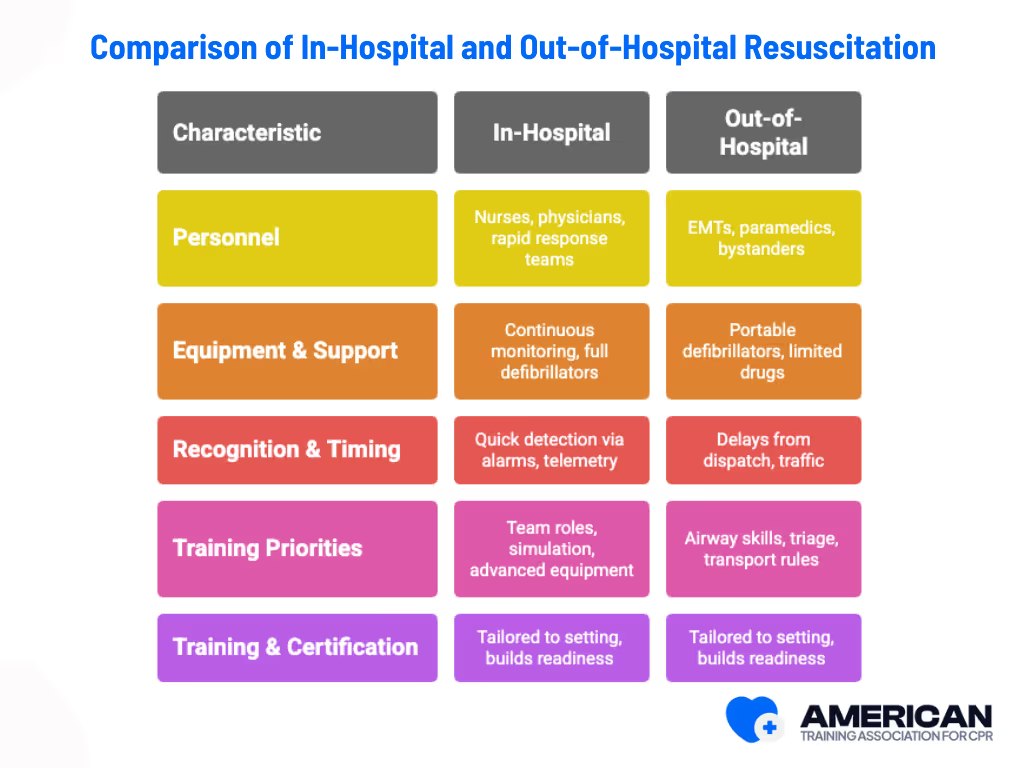
With the 2025 American Heart Association guidelines, the Chain of Survival has been unified for all cardiac arrests (adult, pediatric, neonatal, in-hospital, and out-of-hospital). This means that the core principles and priorities are now the same regardless of where the cardiac arrest occurs.
No matter the setting, survival depends on speed, skill, and coordination. And the best way to prepare is through structured, accredited CPR training. ATAC’s online CPR certification equips healthcare professionals and responders with the knowledge and confidence to act effectively in both hospital and prehospital emergencies.
Disclaimer: Acceptance of online certification may vary depending on state regulations, employer requirements, or specific healthcare roles, so it’s important to confirm before enrolling.

CPR certification equips hospital staff with the essential skills, teamwork strategies, and confidence needed to respond effectively to cardiac emergencies. It ensures individuals can act quickly, teams can coordinate smoothly, and institutions maintain consistent standards of care. Key ways certification prepares hospital staff:
By strengthening individual performance, team coordination, and hospital readiness, CPR certification ensures better patient outcomes.





The first responder activates the emergency response system, usually by dialing the hospital code or emergency number. A team leader, often an advanced provider, assigns roles such as compressor, airway manager, and recorder. This mirrors how first responders and EMS personnel operate during out of hospital cardiac arrest but with hospital specific resources and medical professionals.
CPR must start immediately with compressions at 100 to 120 per minute and 5 to 6 centimeters deep. Hands Only CPR is used until ventilation is established. Benchmarks include full chest recoil, minimal interruptions, and a high chest compression fraction. Feedback devices help track compression depth and response times, supporting both in hospital and prehospital emergency care standards.
A nurse or code team member retrieves the defibrillator, attaches defibrillator pads, and delivers shocks for shockable heart rhythms such as ventricular fibrillation. The AHA recommends delivering the first shock within three to five minutes for witnessed collapse. Hospitals may use both manual defibrillators and automated external defibrillators (AEDs) to shorten perishock pauses and improve survival.
After return of spontaneous circulation, post arrest care focuses on airway stabilization, hemodynamic support, and monitoring. Treatments may include targeted temperature management with fever prevention, coronary angiography, or cardiac catheterization. Patients are usually transferred to intensive care for ongoing management of post cardiac arrest syndrome.
Training combines Basic Life Support (BLS), advanced cardiac life support (ACLS), and simulation drills. Hospitals use training and retention strategies like mock codes, debriefs, and scenario based learning. Certification through an AHA Training Center or Red Cross ensures alignment with global resuscitation guidelines. Regular practice strengthens confidence and response efficiency.
Dispatcher-assisted CPR is primarily a prehospital strategy. In hospitals, the focus is on rapid team activation and code response, while clear EMS-to-hospital communication ensures smooth handoff when patients arrive from the field.
Both the American Heart Association and the European Resuscitation Council publish updated resuscitation guidelines. These guidelines standardize CPR performance, AED use, and post cardiac arrest care across hospitals worldwide. Hospitals that adopt these protocols ensure their staff follow evidence based practices validated by resuscitation conferences and registries like the Cardiac Arrest Registry to Enhance Survival.







