A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
Here is another list:

The Pediatric Chain of Survival is a system of care designed to improve survival after cardiac arrest in infants and children. Most pediatric arrests begin with breathing problems that quickly lead to cardiac arrest, making early recognition and prompt action critical. The chain emphasizes quick identification of emergencies, immediate cardiopulmonary resuscitation with rescue breaths, timely defibrillation when needed, advanced medical care, and specialized hospital treatment. Each step builds on the other, and delays can lower a child’s chance of recovery.
With the American Heart Association 2025 updates, the Pediatric Chain of Survival is now unified with the adult chain, meaning the overall framework and priorities for intervention are the same across all ages. While technical adjustments, such as compression depth and weight-based medication dosing, remain age-specific, caregivers, teachers, healthcare providers, and community members can follow the same unified chain to give children the best chance of survival and long-term health.
The American Heart Association’s 2025 updates unified the Chain of Survival for all ages. The five essential links are:
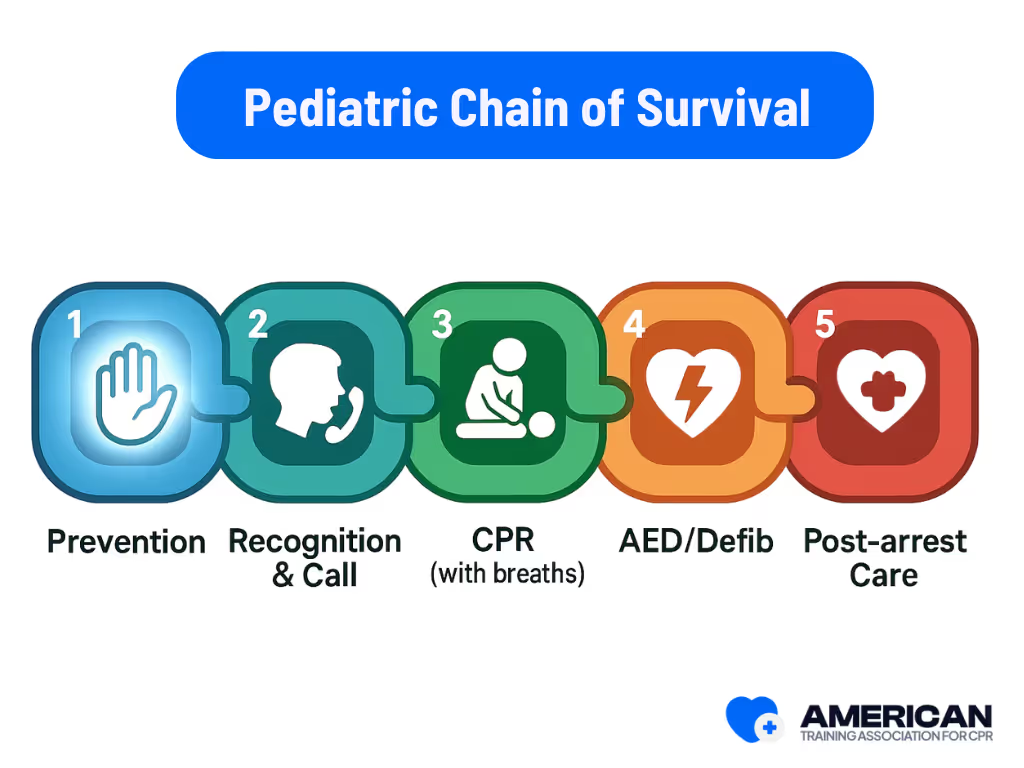
The Pediatric Chain of Survival applies across homes, schools, EMS systems, and hospitals, ensuring children get rapid and continuous care at every stage. It also guides training programs, certification standards, and emergency response protocols so that caregivers, first responders, and healthcare providers know exactly what to do.
Each link in the chain depends on the previous one. Delays or gaps can lower the chances of survival. The next section will outline the five links in the Pediatric Chain of Survival in more detail.





Preventing pediatric cardiac arrest focuses on infectious disease control, injury prevention, and early recognition of clinical deterioration. Prevention lowers incidence and improves survival by stopping children from reaching the point where resuscitation is required.
Children are vulnerable to arrest from illness, injuries, and chronic conditions. Examples include septic shock, airway obstruction, and decompensated congenital heart disease. Timely prevention reduces these risks and strengthens outcomes.
Routine pediatric checkups and immunizations (e.g., influenza, pneumococcal) protect baseline health and lower the risk of severe infections. Chronic disease management plans for asthma or congenital heart disease should outline medication regimens, warning signs, and thresholds for emergency care. Caregivers should also watch for red flags like persistent high fever, poor feeding, or increased breathing effort that may lead to respiratory failure or shock.
Practical measures reduce trauma-related arrests:

Caregivers should be trained to recognize deterioration and respond quickly. Skills include:
Schools, daycare centers, and public health programs strengthen prevention with standardized illness rules, care plans for high-risk children, and rapid access to care. Policies should support clear communication, pediatric medication protocols (e.g., intramuscular epinephrine for anaphylaxis), and efficient urgent-care pathways.
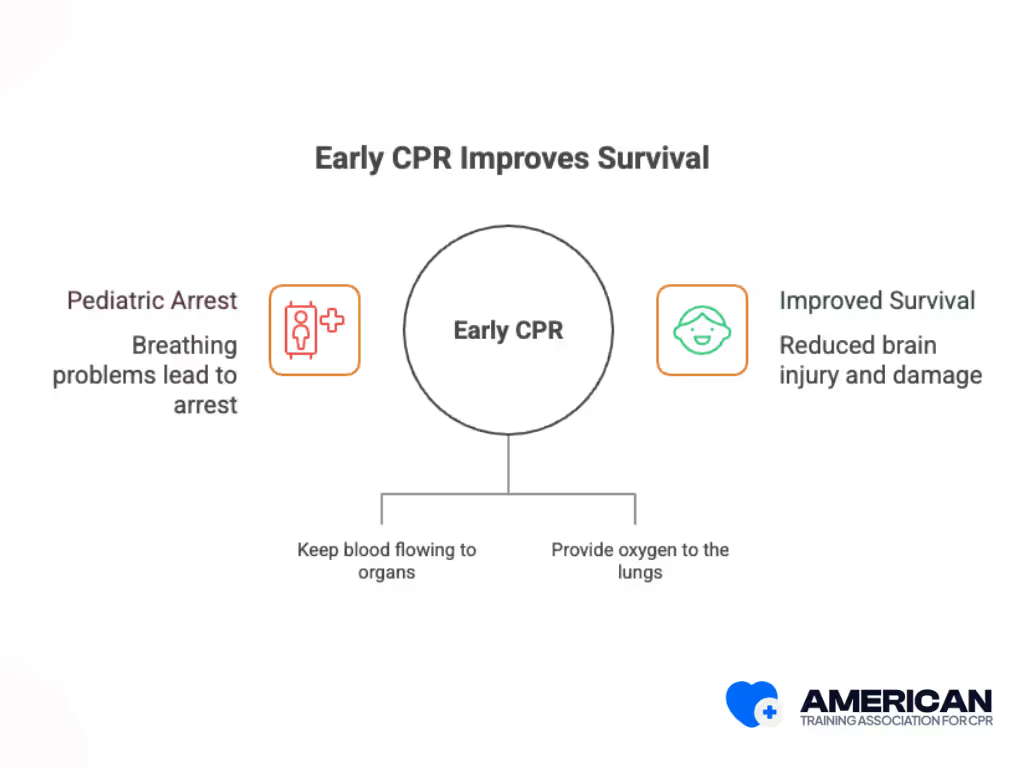
Early CPR is the immediate delivery of chest compressions and rescue breaths to support circulation and oxygenation. It is the second link in the Pediatric Chain of Survival, bridging prevention efforts and advanced therapies until emergency responders arrive.
Pediatric cardiac arrests are often caused by respiratory failure, not heart disease. Early CPR provides life-saving circulation and oxygen delivery, buying time until advanced life support becomes available.
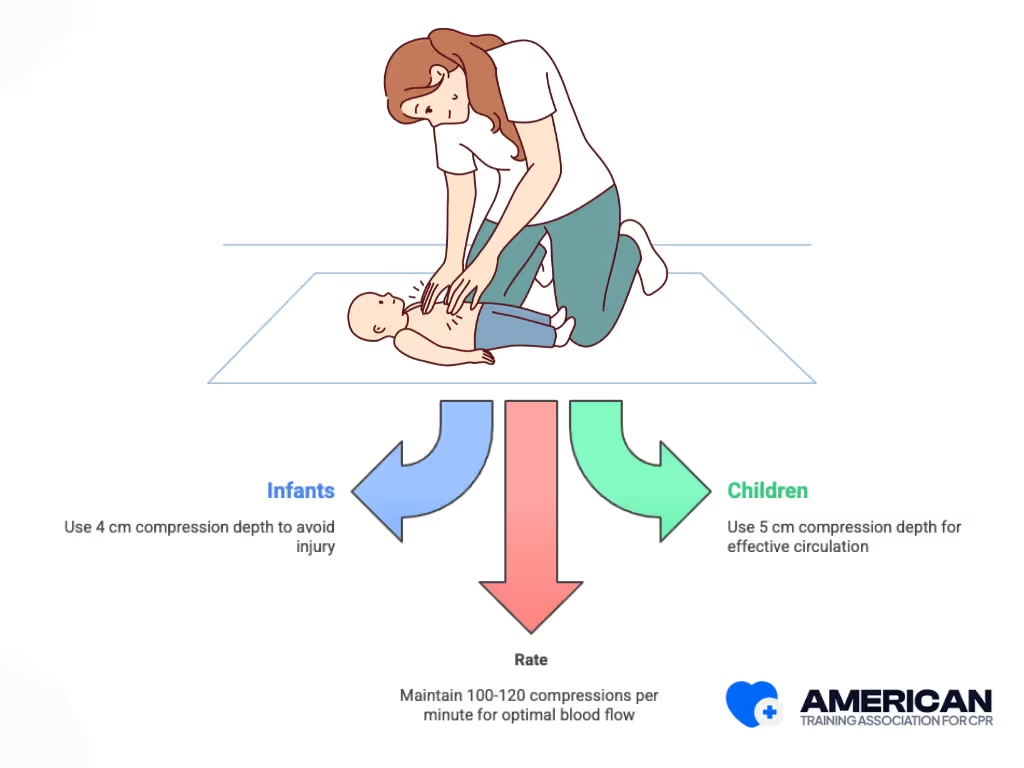
The recommended rate is 100–120 compressions per minute, the same as in adult CPR, to maintain effective blood flow.
Pediatric CPR differs from adult CPR because children usually arrest from breathing problems rather than heart attacks. Infants require two fingers for a single rescuer or two thumbs with encircling hands for two rescuers, while children need one or two hands depending on chest size. Ventilations are also more critical in pediatric cases than in adults.
High-quality compressions, timely ventilations, and proper technique are the foundation of Early CPR in children. These actions keep blood and oxygen flowing until Rapid EMS Activation.
Rapid activation of emergency medical services (EMS) means calling professional responders immediately. This step connects bystander care with paramedic advanced life support and hospital treatment. Any delay weakens the chain of survival.
Call EMS right away if a child is unresponsive, not breathing normally, has severe breathing difficulty, major trauma, or sudden collapse. Always state clearly that the child is unresponsive or not breathing.
Barriers like uncertainty, fear of overreacting, lack of phone access, or language issues can delay the call. These can be overcome by assigning someone to call, keeping emergency numbers on speed dial, enabling emergency phone features, and sharing location via maps or apps.
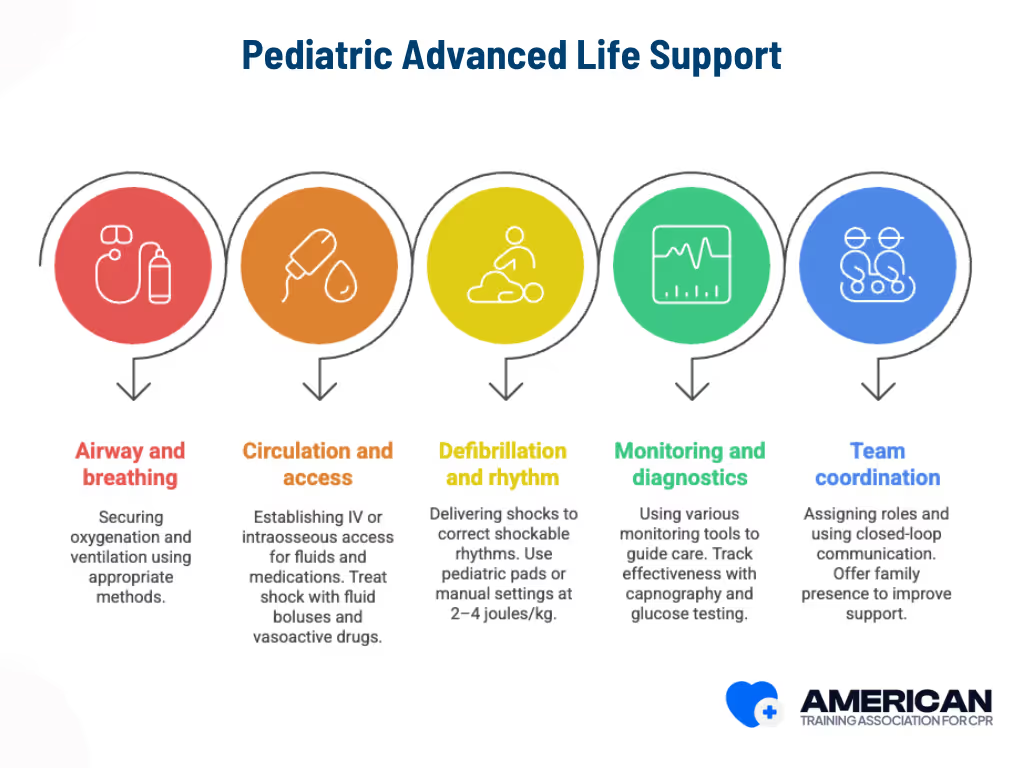
Effective Advanced Life Support (ALS) is the set of advanced interventions performed by trained emergency clinicians to stabilize a child after cardiac arrest, treat reversible causes, and maintain organ perfusion. The goal is to restore circulation and protect neurological function. This step shifts care from bystanders to professionals who can provide definitive treatments.
ALS must be tailored to children because their airway anatomy, body size, and physiology differ from adults. Providers must adjust device selection, medication doses, and techniques to match pediatric needs. Key components of pediatric ALS include:
Because errors in drug dosing or device sizing can cause harm, providers use pediatric weight-estimation tapes and frequent reassessments to minimize risk.
These interventions stabilize the patient, correct reversible causes, and prepare for Integrated Post–Cardiac Arrest Care.
Integrated post–cardiac arrest care in children is a coordinated approach to stabilize and support recovery after return of circulation. The main goals are to maintain physiologic stability, protect the brain and organs, and guide the child toward recovery in the pediatric intensive care unit (PICU).
After a child’s heartbeat is restored, post–cardiac arrest care helps stabilize the body and protect the brain.
The five links work together as a chain. Prevention lowers the number of cases, CPR sustains life, EMS activation ensures continuity, advanced life support stabilizes the patient, and post-arrest care supports recovery. Each link is essential, and gaps in one reduce the effectiveness of the others.






The adult and pediatric chains of survival share the same goal: preventing death from cardiac arrest. However, recent updates from the American Heart Association (2025) have unified the Chain of Survival for all ages, meaning the overall steps and priorities are now consistent for adults, children, and even neonates.
CPR certification prepares you for pediatric emergencies by teaching how to recognize airway obstruction, breathing problems, and cardiac arrest, with age-appropriate CPR techniques. It builds decision-making skills for when to prioritize compressions, give ventilations, or use defibrillation, and emphasizes teamwork, communication, and smooth EMS integration. Training also boosts confidence through realistic scenarios and ensures long-term readiness with refreshers and recertification. ATAC's CPR Course combines all these elements, giving learners the knowledge, skills, and confidence to act quickly and effectively in life-threatening situations involving children.
Early CPR keeps blood and oxygen flowing to the brain and heart before medical help arrives, reducing brain injury and improving survival. Since most pediatric arrests begin with breathing problems, quick action prevents oxygen loss from leading to cardiac arrest and organ damage. Immediate chest compressions and rescue breaths buy time until emergency teams take over.
Yes. Any bystander can perform CPR on a child who is unresponsive and not breathing normally. Acting quickly can make the difference between life and death.
The latest 2025 American Heart Association guidelines encourage children as young as 12 years old to learn and perform effective CPR and AED use, empowering more members of the community to respond during emergencies.
Most states have Good Samaritan laws that protect people who act in good faith, so anyone, trained or untrained, is legally allowed to give CPR. Even if you are not formally trained, you should not hesitate to act:
The 2025 updates also highlight ethical considerations for rescuers: act with beneficence by providing aid, minimize harm, respect the autonomy of patients when possible, and ensure fairness in emergency response. Following these principles helps protect both the patient and the rescuer while promoting high-quality care.
Call immediately if a child is unresponsive and not breathing normally. EMS teams can provide advanced life support, transport, and hospital care.
Yes. Medical professionals encourage parents, teachers, and caregivers to train in pediatric CPR and First Aid because early, correct action improves survival rates and patient outcomes.
The American Heart Association publishes pediatric protocols, the Basic Life Support (BLS) curriculum, and instructor resources used by Training Centers to standardize pediatric resuscitation training.
USCPR certification teaches the skills and builds confidence to act fast in emergencies. It also ensures rescuers know how to follow the full pediatric chain of survival.
While it doesn’t replace advanced hospital care, Pediatric CPR certification benefits include stronger skills, greater confidence, and a recognized credential that shows readiness to respond in real emergencies.







