How Can You Recognize Early Warning Signs?
Recognizing early warning signs is key to providing timely mental first aid. Look for emotional, behavioral, and physical indicators, especially when changes persist or cluster over time. Noticing patterns helps guide intervention and referral to professional care.
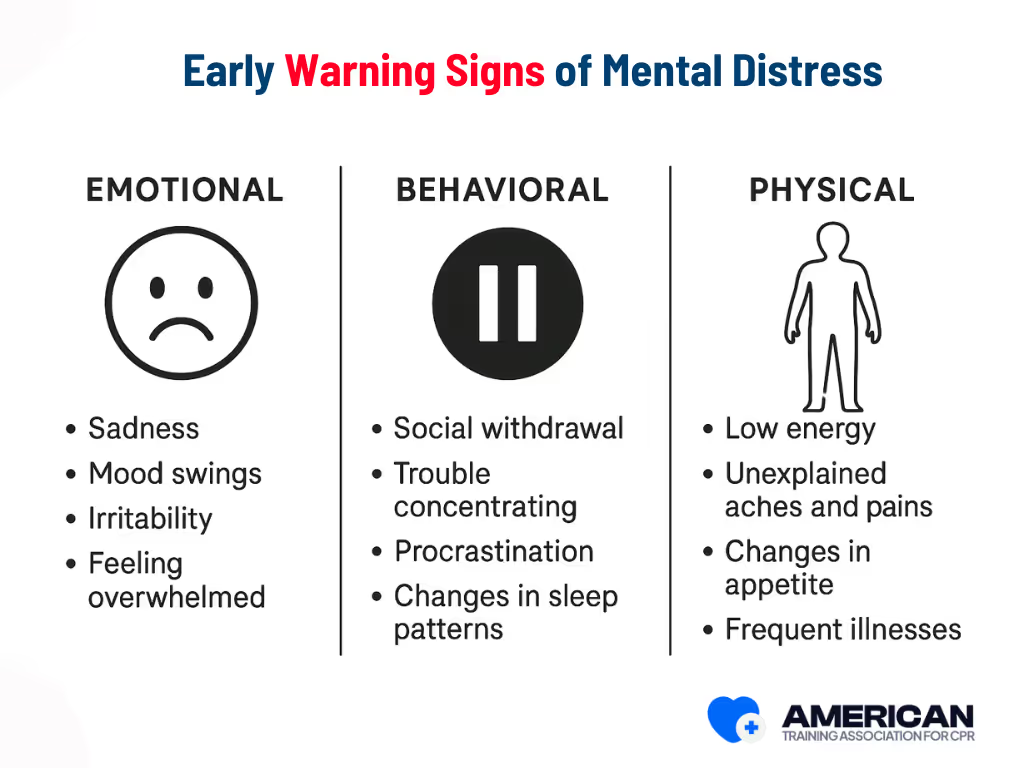
1. Emotional Indicators
Emotional signs include persistent sadness, anxiety, irritability, emotional numbness, or sudden mood swings. For example, someone who usually engages socially may withdraw, or a calm colleague may become unusually tearful or angry. Observe changes relative to their usual baseline, and take seriously any talk of death or suicide, which may require immediate professional help.
2. Behavioral Indicators
Behavioral changes involve shifts in routines or actions, such as social withdrawal, declining work or school participation, poor hygiene, increased substance use, or disrupted sleep and eating patterns. Examples include a student skipping clubs or an employee repeatedly missing shifts. Sudden or risky behaviors often signal the need for early mental health support.
- Social withdrawal or isolation: Avoiding social events, skipping meetings, or reducing contact with friends; may indicate depression or low coping capacity. Respond with a calm check-in, active listening, and practical support.
- Changes in communication or speech: Slurred, rapid, clipped, or unusually paused speech; may signal anxiety, confusion, or substance effects. Slow the interaction, ask simple questions, and assess safety if risk is suspected.
- Agitation or restlessness: Pacing, fidgeting, or repeated movements; can reflect panic or distress. Provide a quiet space, guide grounding techniques, and reduce environmental stressors.
- Decline in daily functioning or routines: Missed deadlines, neglected hygiene, or medication lapses; may indicate worsening mental health. Offer practical assistance, help organize tasks, and connect with mental health resources.
3. Physical Indicators
Physical signs can include fatigue, headaches, gastrointestinal issues, weight changes, or frequent minor injuries. These somatic changes often accompany emotional or behavioral distress. For instance, persistent headaches combined with absenteeism or rapid weight loss alongside social withdrawal can indicate underlying mental health concerns. Encourage evaluation for both medical and mental health causes if symptoms persist.
Early warning signs are most meaningful when they cluster or persist over days to weeks. Single or brief indicators warrant observation, while multiple or sustained changes signal a need for timely mental first aid. Recognizing these patterns helps you respond appropriately and prepare for referral to professional support.
How Do You Provide Mental First Aid?
Providing mental first aid involves a clear, step-by-step approach to ensure immediate support, safety, and connection to professional care:
- Assess safety and risk: Quickly identify danger to the person or others, check for suicidal thoughts, self-harm risk, or medical emergencies, and call emergency services if needed.
- Approach calmly and respectfully: Use a steady voice, open posture, and comfortable distance to reduce stress and build trust.
- Establish connection and listen: Use empathetic listening, reflective statements, and gentle open-ended questions to understand the person’s needs.
- Provide practical support: Help meet immediate needs like contacting family, arranging safe transportation, or accessing crisis resources.
- Offer reassurance and normalize reactions: Validate emotions, explain typical stress responses, and preserve personal agency without promising outcomes.
- Encourage professional help: Guide the person toward mental health services, crisis lines, or primary care appointments and assist in connecting them.
- Arrange follow-up and ongoing support: Schedule check-ins, involve supportive contacts with consent, and maintain engagement to reduce isolation.
- Know your limits and seek supervision: Recognize situations beyond your skill, consult supervisors or clinicians, and debrief when necessary to ensure safe, ethical care.
These steps create a structured, adaptable framework to stabilize acute distress, provide immediate help, and connect individuals to longer-term support, while emphasizing safety, empathy, and professional boundaries.
How Should You Approach and Listen?
Approach with clear, respectful intent and use focused listening to create safety and build trust. The goal is to reduce distress and help the person share their needs and accept next steps.
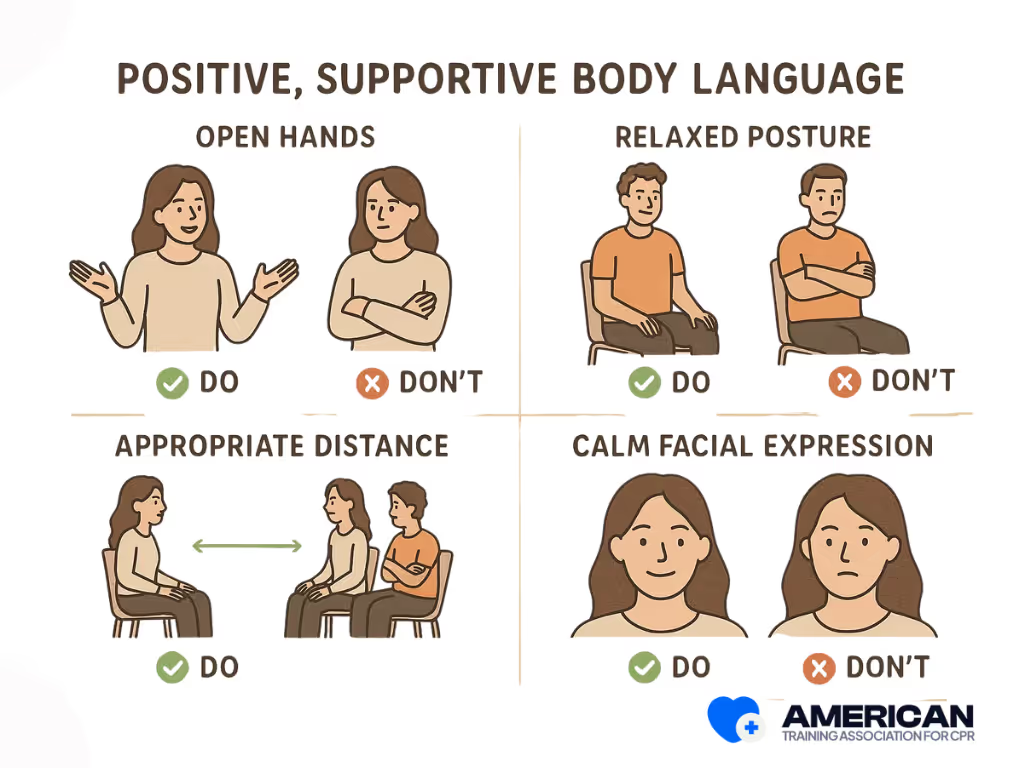
How to approach safely and respectfully?
Move to a comfortable distance of 1 to 2 meters, keep open hands and relaxed posture, introduce yourself, and ask permission to speak or sit. Respecting personal space lowers stress and signals agency. Check the environment for hazards. If there is a weapon, ongoing assault, severe injury, fire, or other danger, stay at a safe distance and call emergency services.
Active listening techniques
Use open-ended questions such as "How are you feeling right now?" or "Can you tell me what happened?" Employ reflective statements like "It sounds like you feel overwhelmed," and allow pauses of 3–5 seconds for responses. Maintain a calm voice, short validation phrases like "I hear you," and minimal encouragers like "mm" or "I see." These techniques build trust, reduce defensiveness, and clarify needs.
Handling difficult responses:
- Silence: Stay present and wait calmly.
- Anger: Set boundaries and stay calm.
- Withdrawal: Offer choices like "I can stay for five minutes or come back later."
Stop if the person asks, or if there are medical or suicidal risks (e.g., severe injury, loss of consciousness, intent to self-harm). Prioritize safety and respect autonomy. This approach creates rapport and safety, paving the way for Providing Reassurance, where you offer comfort, normalize reactions, and guide next steps.
How Do You Provide Reassurance?
Providing reassurance helps reduce distress, lower perceived threat, and restore emotional safety using calm verbal cues, grounding prompts, and controlled body language.
Use reassurance when someone is anxious, panicked, shocked, grieving, or agitated after events like accidents, medical emergencies, or traumatic news. Do not provide reassurance if the person is in immediate danger or situational safety isn’t resolved. Reassurance supports the previous step, Approach and Listen, and usually comes before encouraging professional help.
Do’s:
- Calm tone: Speak slowly and steadily, about 100–130 words per minute.
- Validate feelings: Use phrases like “I hear how upset you are” or “I can see you are frightened.”
- Offer facts: Simple status updates like “You are safe here, help is on the way.”
- Grounding prompts: Ask them to notice five things in the room or practice breathing (inhale 4, exhale 6).
- Ask permission: Check before offering touch or practical assistance.
- Keep it short: Use one- or two-sentence statements.
Don’ts:
- Don’t minimize feelings (e.g., “It’s nothing”).
- Don’t promise outcomes (e.g., “You’ll be fine for sure”).
- Avoid platitudes or complex explanations.
- Don’t blame or judge.
Maintain steady, slow speech, open posture, and empathetic facial expressions. Use concrete, present-focused language like “right now” or “here” to anchor attention. Avoid incongruent signals, such as smiling while rushing through statements.
Encourage Professional Help
When distress is serious or persistent, guide the person to licensed mental health care. Professionals can assess, diagnose, and provide therapy or medication. Escalate when there’s suicidal intent, lasting symptoms, severe withdrawal, or sudden mood changes.
- Calmly note behaviors and express concern.
- Offer concrete options and ask permission to assist.
- Address barriers like stigma, cost, or transportation.
- Provide resources: clinics, telehealth, counseling services, or crisis lines (e.g., 988 in the U.S.).
Encouraging professional help connects immediate support to long-term care and ensures the person receives the help they need.
Self-Care for the Helper
Providing mental first aid can be emotionally demanding, so self-care is essential to maintain effectiveness and prevent burnout. Key steps include:
- Take a short pause: Step aside for a few minutes to regain composure.
- Ground yourself: Use breathing exercises or sensory anchors to reduce stress.
- Check safety and boundaries: Ensure the situation remains safe and within your role.
- Seek support: Debrief briefly with a colleague or supervisor.
- Record notes: Log observations, actions, and referrals to clear your mind.
- Rehydrate and refuel: Drink water and have a light snack to restore energy.
- Schedule a debrief: Plan a longer follow-up discussion within 24–72 hours.
- Monitor mood and sleep: Track changes for one to two weeks for early signs of stress.
- Use formal supports: Contact an EAP, peer network, or occupational health service if needed.
- Plan restorative activities: Take short walks, do relaxation exercises, or enjoy a hobby.
Self-care protects your wellbeing so you can continue providing effective mental first aid.
Common Misconceptions About Mental First Aid
Mental First Aid (MFA) is often misunderstood. Correcting these myths helps responders use it safely and effectively.
- Only professionals can provide it: Trained community members can offer support, recognize distress, and guide individuals to professional care.
- It replaces therapy: MFA is first-response support, not a substitute for formal treatment. It connects people to ongoing care.
- Certification is required: Brief standardized courses equip nonclinicians with practical skills like active listening and safety planning.
- It always deescalates crises: MFA helps reduce distress but cannot guarantee safety in every high-risk situation. Emergency services must be activated when danger exists.
- It’s only for disasters: MFA applies in everyday settings, including workplaces, schools, and homes, to manage routine stress and prevent escalation.
Understanding these myths ensures proper use of Mental First Aid and improves outcomes.
Special Considerations for Different Groups
Mental health first aid (MHFA) should be adapted for different populations, considering communication style, assessment cues, consent, cultural factors, and referral options. Key groups include children and adolescents, older adults, workplace populations, culturally and linguistically diverse communities, LGBTQ+ individuals, people with substance use disorders, refugees and asylum seekers, and people with disabilities.
Children and Adolescents (0–18 years):
- Involve parents or guardians when safe.
- Match communication to developmental level: simple sentences for preschoolers, visual tools for school-age children, collaborative dialogue for teens.
- Look for behavioral cues like regression, academic decline, or somatic complaints.
- Follow mandatory reporting rules for abuse or harm.
- Adapt core MHFA steps (approach, listen, reassure, encourage professional help) to include caregiver consent and age-appropriate strategies.
Older Adults (65+ years):
- Account for sensory or cognitive changes; check hearing, vision, and comprehension.
- Review medications and medical events that may mimic psychological symptoms.
- Watch for atypical signs like withdrawal, falls, or confusion.
- Include caregivers and proxies in consent and follow-up planning.
- Address mobility or transportation barriers when arranging professional care.
Workplace Populations:
- Respect confidentiality and company policies.
- Clearly separate peer support from professional mental health roles.
- De-escalate safely in shared spaces; use private rooms or call security if needed.
- Signpost employee assistance programs, temporary adjustments, or accommodation options when functional impairment is observed.
Other Subgroups:
- Culturally and linguistically diverse communities: use interpreters, translated materials, and culturally adapted screening.
- LGBTQ+ individuals: use affirmed names and pronouns; connect to identity-affirming services.
- People with substance use disorders: prioritize overdose recognition, harm reduction, and nonjudgmental referral.
- Refugees and asylum seekers: use trauma-informed approaches, avoid retraumatizing questions, and provide legal and psychosocial referrals.
- People with disabilities: provide accessible materials, support assistive devices, and offer interpreters or tactile/large-print resources.
Tailoring MHFA to population-specific needs improves effectiveness and ensures safe, respectful support.
Why You Should Take First Aid Training
First aid training equips you to respond quickly and effectively in emergencies, covering essential skills like CPR, airway management, bleeding control, and safe use of tools such as tourniquets. Through simulations, role-plays, and structured exercises, learners practice decision-making under pressure and learn to recognize life-threatening situations within seconds, ensuring timely intervention and reducing harm. Courses also teach standardized handover methods like MIST or SBAR, improving communication with emergency responders.
Beyond immediate care, training builds confidence, psychological readiness, and community resilience. Participants gain hands-on experience, learn legal protections, and understand their role in workplace or public safety. While first aid does not replace professional medical services, it allows bystanders to stabilize patients, limit secondary injury, and support emergency teams effectively, making trained responders a vital part of public safety.




.avif)