Must-Have Wilderness First Aid Kit Items
A wilderness first aid kit is a carefully selected set of medical supplies used to stabilize and manage injuries and medical issues in remote outdoor settings until professional help arrives. The kit focuses on hemorrhage control, airway and breathing support, fracture immobilization, infection prevention, environmental protection, and basic medications.
- Sterile Dressings: Protect open wounds, control bleeding, and reduce infection risk. Include trauma pads of multiple sizes and non-adherent dressings for burns. Keep sealed until use.
- Bandages and Adhesive Tape: Secure dressings, support sprains, and maintain compression. Include elastic and non-elastic bandages and hypoallergenic tape.
- Hemostatic and Bleeding-Control Adjuncts: For severe bleeding not controlled by standard dressings. Include a hemostatic dressing and a windlass tourniquet, and ensure proper training.
- Wound-Cleaning Supplies: Reduce infection risk by irrigating and prepping wounds. Include sterile saline, chlorhexidine or povidone-iodine swabs; avoid hydrogen peroxide for routine use.
- Splinting and Immobilization Materials: Stabilize fractures and joint injuries. Include rigid splints, SAM-type splints, and triangular slings. Practice proper immobilization techniques for safe evacuation.
- Burn Care Supplies: Protect and treat burns. Include sterile non-adherent dressings, hydrogel sheets, or foil-backed burn sheets. Avoid ice and do not break blisters.
- Thermal Protection and Emergency Shelter: Maintain core temperature and prevent hypothermia. Include space blankets, emergency bivy or tarp, insulating pads, and warm clothing.
- Personal Protective Equipment (PPE): Protect responders from blood or bodily fluids. Include disposable gloves, face shield, and eye protection. Dispose of used items safely.
- Analgesics and Basic Medications: Provide pain relief, fever reduction, and hydration. Include acetaminophen, ibuprofen, and oral rehydration salts. Clearly label all medications.
- Allergy and Asthma Emergency Items: Support patients with severe allergic reactions or asthma. Include epinephrine auto-injectors and short-acting bronchodilator inhalers. Train all users on proper use.
- Tools and Instruments: Assist with wound care and splinting. Include trauma shears, tweezers, penlight, and a small thermometer. Keep instruments clean and secured.
- Suture and Wound-Closure Alternatives: Temporarily close minor lacerations. Include sterile adhesive strips or medical-grade tissue adhesive for trained users. Avoid use on contaminated wounds.
- Navigation and Communication Aids: Enable signaling and evacuation. Include a map, compass, whistle, personal locator beacon, or satellite messenger with charged batteries.
- Personal Items and Medical Documents: Inform responders of allergies, medications, and health conditions. Include waterproof copies of medication lists, insurance, emergency contacts, and encourage medical ID bracelets.
These items collectively prepare responders to manage common wilderness injuries and medical emergencies, including bleeding, fractures, burns, allergic reactions, and environmental exposure, until evacuation or professional medical care is possible. Kit contents should be tailored to trip duration, environment, and participant needs.
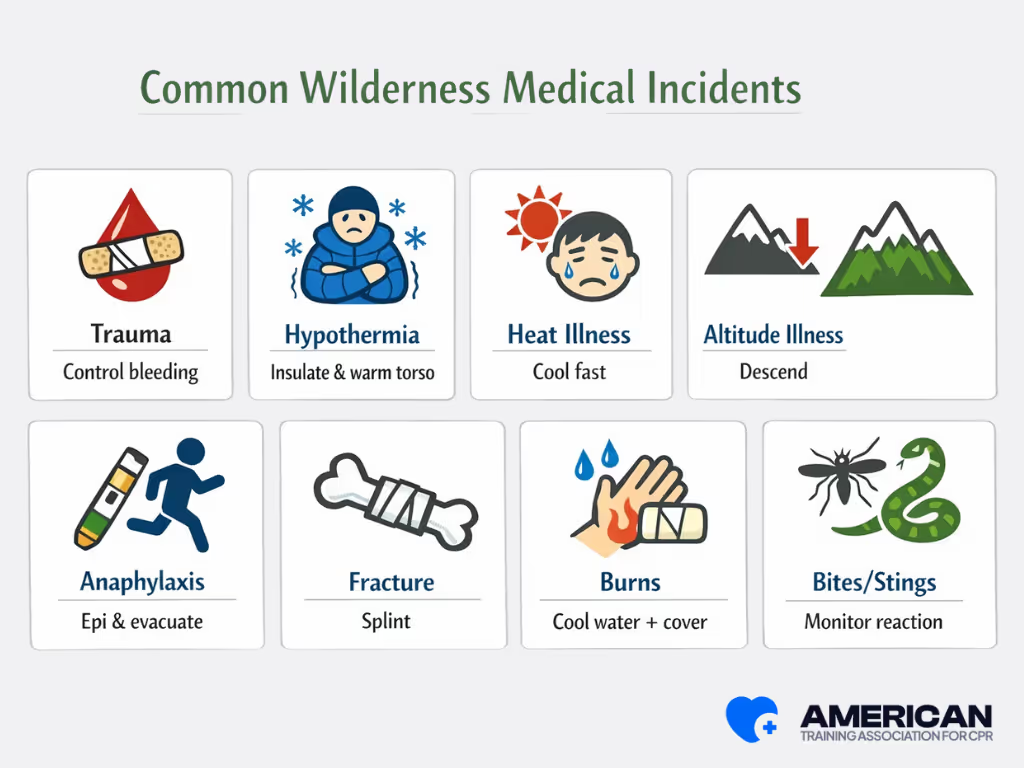
What are the Common Wilderness Injuries and How to Treat Them?
In the backcountry, medical responders frequently encounter lacerations, burns, fractures, bites/stings, and altitude-related illness. Proper field management focuses on stabilizing the patient, preventing complications, and preparing for evacuation when needed.
1. Cuts and Lacerations
Cuts and abrasions are common injuries that require bleeding control and contamination prevention.
- Bleeding control: Apply direct pressure with a clean dressing for at least 10 minutes. Elevate the limb if no fracture is suspected and use a pressure bandage for arterial bleeding.
- Wound cleaning: Irrigate with 500 ml of potable water or sterile saline, removing visible debris with forceps and sterile gauze. Avoid tissue-damaging antiseptics unless advised.
- Dressing and monitoring: Apply sterile or non-adherent dressings and change every 24–48 hours. Watch for pain, redness, swelling, or pus.
Seek suturing within 6–12 hours for facial or joint wounds. Evacuate immediately for deep wounds, exposed tendons, uncontrolled arterial bleeding, or signs of infection.
2. Burns
Burns can be thermal, chemical, or solar. Treatment focuses on cooling, analgesia, and protection.
- Cooling: Irrigate burns with cool potable water for 10–20 minutes; prevent hypothermia in cold environments.
- Pain control: Administer oral analgesics (ibuprofen 400 mg or acetaminophen 500–1000 mg) and monitor vital signs every 15 minutes.
- Dressing: Cover burns with sterile, non-adherent dressings or clean dry sheets.
- Evacuation: Seek care for burns >10% total body surface area, full-thickness burns, facial/airway burns, or chemical/electrical burns.
3. Fractures
Fractures and dislocations require immobilization and pain management.
- Assessment: Check for open vs. closed injuries, distal pulses, capillary refill, and sensation.
- Splinting: Immobilize the limb in the position found with rigid materials and secure joints above and below the injury.
- Transport support: Use slings, vacuum, or improvised splints. Provide oral analgesia and monitor for shock.
- Evacuation: Immediate evacuation for open fractures, compromised circulation, neurological deficits, or joint dislocations that cannot be reduced safely.
4. Bites and Stings
Animal and insect bites require wound care, envenomation assessment, and infection prevention.
- Wound care: Clean with 200–500 ml potable water, remove stingers with a flat object, immobilize limb if venomous.
- Severe signs: Watch for respiratory distress, hypotension, swelling, or neurotoxic effects. Monitor vital signs frequently.
- Allergic reactions: Administer intramuscular epinephrine (0.3 mg adults) for anaphylaxis and repeat every 5–15 minutes if needed while arranging evacuation.
- Infection: Consider antibiotics for human/cat bites or infected wounds.
- Remote setting considerations: Lower thresholds for evacuation due to limited antivenom or specialist care.
5. Altitude-Related Illness
Altitude sickness requires descent and symptomatic management.
- Recognition: Mild acute mountain sickness presents with headache plus nausea, insomnia, or dizziness. High-altitude pulmonary edema shows dyspnea at rest and cough. Cerebral edema may cause ataxia or altered mental status.
- Immediate measures: Descend 300–500 meters, provide supplemental oxygen (2–6 L/min), and administer acetazolamide (125–250 mg every 12 hours) or dexamethasone (4 mg every 6 hours) as needed.
- Supportive care: Rest, hydration, and analgesia for mild cases. Urgent evacuation for progressive dyspnea, reduced consciousness, or failure to improve after descent.
Common Principles Across Injuries
Effective wilderness care also relies on:
- Scene safety: Use PPE to reduce provider risk.
- Infection prevention: Use sterile dressings, potable water, and ensure tetanus immunization is up to date.
- Pain management: Provide measured oral analgesics and document doses.
- Continuous reassessment: Monitor airway, breathing, and circulation every 15–60 minutes to guide interventions and evacuation decisions.
By following these protocols, responders can stabilize patients, prevent deterioration, and prepare for evacuation, while prioritizing safety and practical care in austere backcountry environments.
.avif)